That sharp, radiating pain in your back is more than just a nuisance; it’s a direct signal from your body trying to tell you something’s wrong. Often, a herniated disc is the culprit, and finding lasting relief usually means gentle, hands-on therapies that focus on restoring your body's natural function—without resorting to invasive procedures.
Understanding Disc Herniation and Finding Relief

To get a clear picture of what’s happening inside your spine, think of your spinal discs as little jelly doughnuts stacked between your vertebrae. The doughnut part is the tough, fibrous outer casing (the annulus fibrosus), while the jelly is the soft, gel-like centre (the nucleus pulposus). When you have a herniated disc, a tear in that tough outer layer allows some of the jelly to squeeze out.
This is where the trouble starts. That leaked material can press directly on the highly sensitive nerves running along your spinal column. It’s this pressure that triggers the debilitating symptoms so many people experience, like sciatica or a relentless ache in the lower back. Your body is sending a very clear distress signal that something is mechanically out of place.
The Impact on Your Body
The consequences of this nerve pressure can seep into every part of your life. Simple movements we take for granted, like bending down to tie your shoes or even just sitting for a while, can become intensely painful. This isn't just a minor ache; it's a structural problem that demands a targeted solution.
The good news is that conservative, drug-free approaches are often the first and most effective line of defence. These methods are all about:
- Restoring proper movement: Gentle, targeted adjustments can help take the pressure off the irritated nerve.
- Reducing inflammation: By improving how the joints move, we help the body’s natural healing processes work more efficiently.
- Improving overall function: The real goal is to correct the underlying issue, not just to mask the symptoms with medication.
It’s a common mistake to think all back pain is the same. But a herniated disc creates a very specific type of nerve irritation that requires a precise, hands-on approach to resolve. Getting to the root mechanical cause is the absolute key to achieving lasting relief.
To help you recognise the signs, here's a quick guide to what a herniated disc might feel like.
Herniated Disc Symptoms at a Glance
Use this quick guide to recognise the common signs associated with a herniated disc and understand what your body might be telling you.
| Symptom | What It Feels Like | Commonly Affected Area |
|---|---|---|
| Radiating Pain | A sharp, shooting, or burning pain that travels from your back down your leg. | Buttocks, back of the thigh, calf, and even the foot. |
| Numbness or Tingling | A "pins and needles" sensation or a loss of feeling in the affected limb. | Arms, hands, legs, or feet, depending on the disc. |
| Muscle Weakness | Difficulty lifting objects, stumbling, or feeling like a limb might "give way." | The muscles controlled by the affected nerve. |
| Localised Back Pain | A persistent dull ache or sharp pain centred around the site of the herniation. | Lower back (lumbar) or neck (cervical) region. |
Remember, these symptoms can vary from person to person, but if any of them sound familiar, it’s a good sign to get a professional opinion.
The Path to Recovery
Lumbar disc herniation affects about 1 in 1,000 people annually in the UK, and for around 85% of those affected, lower back pain is the main symptom. Its prevalence is why so many people seek out specialised manual care, which offers natural, non-invasive treatments designed to relieve nerve pressure and get you moving properly again.
For another perspective on managing chronic pain, particularly with back issues, it can be useful to explore insights on getting out of pain via the mind-body connection. This viewpoint complements physical therapies by acknowledging the psychological side of discomfort. Ultimately, the aim is to find a sustainable way forward. If you're ready to explore how targeted manual therapies can address a herniated disc, our team is here to help you understand your options.
Learning to Read Your Body's Warning Signs

It’s all too easy to brush off back pain. We blame it on a tough workout, a long day slumped over a desk, or just sleeping awkwardly. But the discomfort from a herniated disc is different—it sends out very specific signals that go well beyond a simple ache. Learning to tune in to these warnings is the first real step towards getting the right kind of help.
Think of it like this: your body has its own language. When a disc presses on a nerve, it doesn't just hurt in that one spot. Instead, it creates a chain reaction all the way down that nerve's path. This is exactly why a problem in your lower back can suddenly make your foot feel tingly or weak. Understanding these connections is key to realising your symptoms are pointing to something more than just tired muscles.
Beyond a Simple Backache
The most telling sign of a disc problem is often radiating pain. This isn’t some vague, dull throb. It’s a sharp, often burning or electric-shock sensation that travels. If the troublesome disc is in your lower back (which is the most common spot), this pain typically shoots down your buttock and into your leg. This is the classic sign of sciatica.
This nerve-related pain feels completely different to muscle soreness. A strained muscle might be tender and stiff in one area, but nerve pain follows a clear, defined path, often causing trouble in places far from the actual issue in your spine.
This can show up in a few distinct ways:
- Sharp, travelling pain: A jolt down the back of your thigh or calf when you cough, sneeze, or strain.
- Constant, burning ache: A deep, persistent ache along the nerve pathway that just doesn’t seem to ease up, even with rest.
- Pins and needles: That nagging tingling or numb sensation, like a limb has "fallen asleep," but the feeling stubbornly refuses to go away.
When Symptoms Interfere with Daily Life
These aren't just abstract feelings; they have a real impact on your day-to-day life. The discomfort can turn simple actions into painful challenges. You might start noticing the effects of a disc herniation when you struggle with tasks that you once did without a second thought.
Do any of these scenarios sound familiar?
- Difficulty getting up: Do you need to use your arms to push yourself out of a chair because of a shooting pain?
- Trouble with balance: Are you finding yourself stumbling or feeling unsteady on your feet due to weakness or numbness in one leg?
- Loss of grip: If the disc issue is in your neck, you might suddenly struggle to hold a coffee mug, a pen, or even a bag of groceries.
The body’s signals are rarely subtle when a nerve is involved. Unexpected muscle weakness or a persistent pins-and-needles sensation are not symptoms to ignore. They are clear indicators that a nerve is being compromised and requires professional attention.
Recognising Red Flag Symptoms
While most disc symptoms can be managed brilliantly with conservative care, there are a few "red flag" symptoms that need immediate medical attention. These are signs of a more serious type of nerve compression that could lead to permanent damage if not dealt with quickly.
It is crucial to seek emergency care if you experience any of the following:
- Loss of bowel or bladder control: This is a key sign of a rare but very serious condition called cauda equina syndrome.
- Saddle anaesthesia: Numbness in the areas that would touch a saddle—your inner thighs, groin, and buttocks.
- Progressive weakness: A noticeable and worsening weakness in your legs that makes it difficult to stand up or walk properly.
Recognising these critical signs, alongside the more common symptoms, empowers you to take swift, appropriate action. By becoming an expert in your own body's signals, you can move past the confusion of "just back pain" and get on a clear path towards targeted, effective relief.
How Gentle Manual Therapies Address Disc Pain
When you’re stuck with the nagging, relentless pain of a disc herniation, the last thing you want is aggressive treatment. The real goal is to get to the root of the problem, and that’s where skilled, hands-on care comes in. We use precise and gentle techniques designed to relieve pressure, restore healthy movement, and kick-start your body’s own healing process.
This isn't about forceful cracking or twisting. It’s about controlled, specific actions that target the exact spinal segments causing you trouble. The focus is on creating subtle but powerful changes that give the irritated nerve and damaged disc the space they need to recover.
Creating Space and Relieving Pressure
One of the most effective methods we use is a gentle, non-force technique known as flexion-distraction. This involves a specialised table that moves in a very specific way to carefully stretch and decompress the spine. By gently separating the vertebrae around the herniated disc, we can create a tiny bit of negative pressure—almost like a subtle vacuum effect—inside the disc itself.
That vacuum is the key. It helps to gently draw the bulging disc material back towards the centre, pulling it away from the sensitive nerve it’s been pressing on. This simple action can bring almost immediate relief from radiating pain like sciatica because it takes the pressure right off the source of the irritation.
Imagine a compressed sponge that's been deprived of water. Gentle manual therapies act like a slow, steady rehydration process, helping the spinal disc regain its natural space, absorb vital nutrients, and reduce the painful pressure on surrounding nerves.
This decompression doesn't just help reposition the disc; it also dramatically improves circulation. Better blood flow brings oxygen and nutrients to the damaged tissues while flushing away the inflammatory chemicals that fuel the pain. Creating this healthier environment is absolutely crucial for genuine, long-term healing.
Restoring Proper Spinal Movement
Another cornerstone of our approach is spinal mobilisation. This technique involves slow, passive movements applied to the spinal joints. Unlike a high-velocity adjustment, mobilisation is a much gentler process aimed at increasing the range of motion in joints that have become stiff or "stuck."
When a disc herniates, the surrounding muscles instinctively tighten up to guard the injured area, which leads to stiffness and dysfunctional movement patterns. Spinal mobilisation helps to gently break this painful cycle by:
- Improving joint flexibility: It carefully moves the joints through their natural range, easing away stiffness.
- Reducing muscle spasm: The gentle, rhythmic movements help convince tight, overactive muscles to finally relax.
- Restoring nerve function: By correcting misalignments and improving movement, it ensures nerve signals can travel freely without interference.
This infographic shows how a combination of different techniques all work together towards a successful recovery.
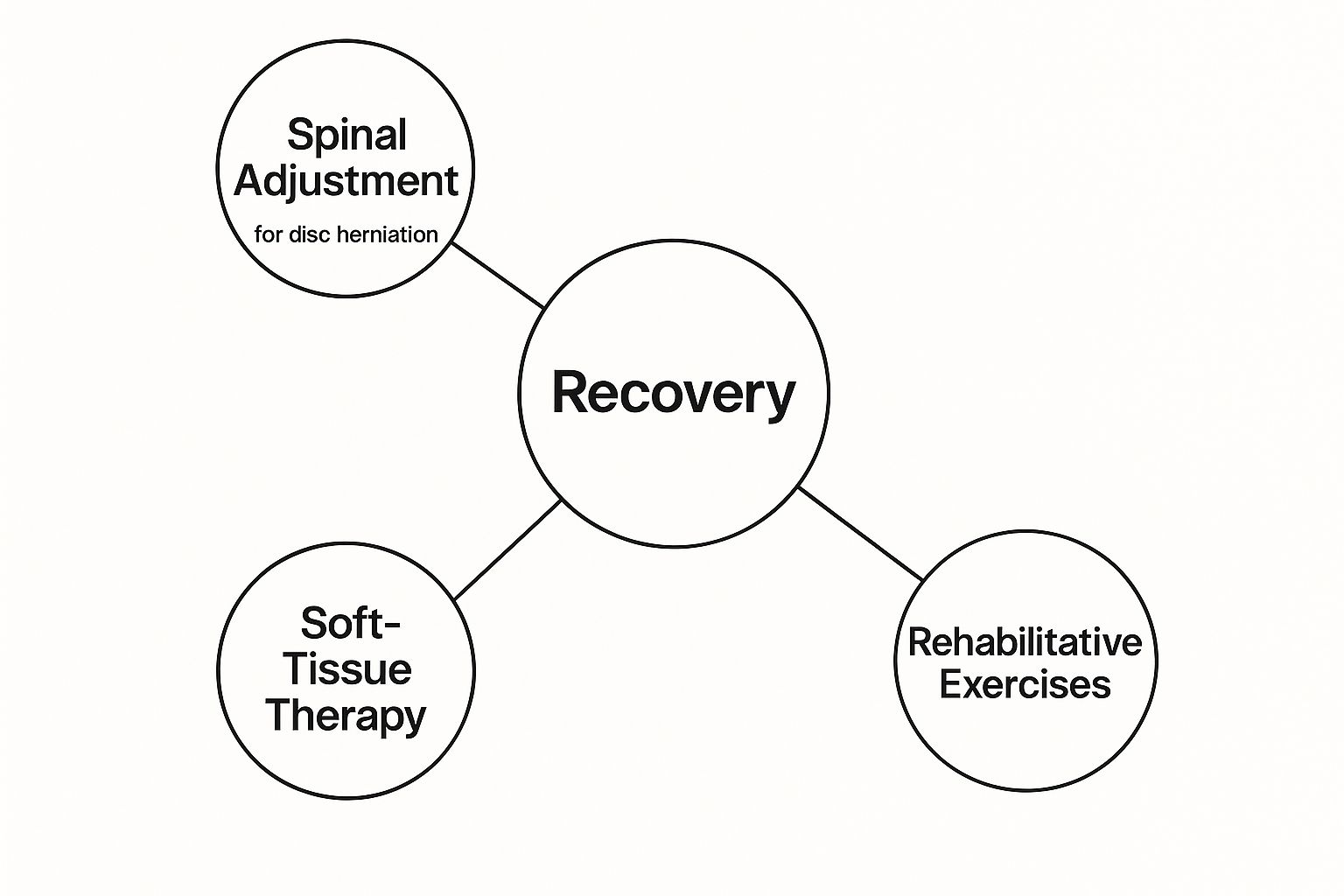
As you can see, a successful outcome often depends on a multi-faceted approach. We combine hands-on adjustments with other supportive therapies to make sure we’re addressing every aspect of the injury.
A Personalised Path to Recovery
No two disc herniations are ever the same. A skilled practitioner knows this and will develop a care plan specifically for your unique diagnosis, symptoms, and health goals. Your treatment will always be based on a thorough assessment of your condition, not a one-size-fits-all protocol.
This personalised approach might also include other supportive therapies. For example, soft tissue therapy can be used to release tight muscles and trigger points that are contributing to your pain and poor posture. We’ll also guide you through targeted rehabilitative exercises to strengthen your core and stabilise your spine—an essential step for preventing future flare-ups.
Understanding the differences between manual therapy disciplines can also be helpful. To learn more, you might find our guide exploring the differences between specialised spinal care and physiotherapy useful. By combining these careful, hands-on techniques with a plan tailored specifically to you, it's possible to move beyond just managing symptoms and start on a genuine path to lasting recovery.
Of course. Here is the rewritten section, crafted to sound like an experienced human expert while preserving all the original information, links, and formatting.
Does Chiropractic Treatment for Herniated Discs Really Work?
So, Does This Stuff Actually Work? A Look at the Evidence
When you’re in pain, there’s only one question that really matters: will this treatment help me? It’s completely normal to feel a bit sceptical, especially when you’re thinking about a non-surgical path for something as serious as a disc herniation. The good news is that a solid body of clinical evidence shows that specialised manual therapies aren’t just effective—they can be a powerful first line of defence against more invasive procedures.
Many people think surgery or a long-term prescription are the only real options for a herniated disc. But a growing pile of research is pointing in another direction, backing conservative care as a smart primary strategy. These studies aren’t just theoretical; they focus on real-world outcomes. Do patients get better? Can they get back to their normal lives? And, crucially, can they avoid going under the knife?
What the Clinical Outcomes Tell Us
The success of hands-on spinal care isn't just based on feel-good stories; it's backed by hard data. Study after study has looked at how these treatments affect pain levels, a person's ability to function day-to-day, and the long-term need for surgery. The findings are compelling, showing significant improvements for most patients who choose this route.
A lot of the research zooms in on lumbar disc herniation (LDH) with radiculopathy. That’s the technical term for a slipped disc in the lower back that sends pain shooting down the leg, otherwise known as sciatica. It’s one of the most common and miserable forms of disc injury, which makes it a critical area of focus.
The bottom line is that getting to the mechanical cause of the disc pain with skilled, hands-on care can lead to substantial, lasting relief. It shifts the focus from just masking symptoms to actually correcting the underlying problem—and that’s the key to long-term spinal health.
This focus on fixing the root cause is why so many people don't just feel less pain, but see a real improvement in their overall quality of life.
The All-Important Link to Avoiding Surgery
Perhaps the most powerful argument for this approach is its track record in helping people avoid the operating theatre. Clinical evidence, including data from right here in the UK, supports spinal manipulation as a safe and effective non-surgical option for lumbar disc herniation. For anyone worried about the risks and lengthy recovery that come with surgery, this is incredibly encouraging news.
In fact, the numbers are pretty remarkable. Studies show that patients who start with this type of care have a much lower chance of needing a lumbar discectomy down the line. One study found a 69% reduction in the odds of surgery after one year, and an even more impressive 77% reduction at the two-year mark compared to patients receiving other treatments. You can discover more about these findings on Chiro-Trust.org.
Statistics like these highlight something huge: choosing a conservative approach first could completely change your recovery journey for the better.
What This Means For You
So, what does all this research mean in simple terms? It means that choosing specialised manual care for a disc herniation is a decision backed by solid evidence. It offers a safe and proven route to relief that could genuinely help you sidestep the need for more aggressive treatments.
Our goal here is to show you the science so you can feel confident in non-surgical care. Think of it as a powerful first step, grounded in proof, towards taking back control from disc pain and getting back to doing the things you love.
Your First Visit: What to Expect From Your Assessment

Taking that first step towards sorting out disc pain can feel a bit intimidating, especially if you’re not sure what happens next. A proper initial consultation isn't just a quick chat; it's a deep dive into figuring out exactly where your pain is coming from. This detailed diagnostic process is the bedrock of any effective, personalised care plan.
The entire visit is designed to build a complete picture of your health. It all starts not with treatment, but with a simple conversation. A thorough, unhurried review of your health history gives you the space to tell your story—when the pain began, what makes it flare up, and how it's getting in the way of your life. This is a vital piece of the puzzle, offering clues that guide the rest of the examination.
The Physical Examination
Once we understand your history, the next step is a detailed physical assessment. This is where a practitioner uses their hands and expertise to evaluate how your body is moving and functioning. The goal is to see how your spine, muscles, and nerves are all working together.
This hands-on examination usually includes several key parts:
- Postural Analysis: How you naturally stand and sit can reveal underlying imbalances that are putting extra stress on your spinal discs.
- Range of Motion Tests: We’ll gently move your spine and limbs to see which movements trigger pain and where your flexibility might be limited.
- Palpation: This simply means carefully feeling the muscles, ligaments, and joints along your spine to find any specific spots of tenderness, tightness, or inflammation.
This hands-on approach gives us immediate feedback about what’s going on physically, helping us look beyond the symptoms to find the real source of the problem.
The initial assessment is all about connecting the dots. It links the symptoms you’re describing—like that shooting leg pain—to specific, observable physical findings. This ensures any care that follows is targeted with precision.
After that, the focus shifts to how the disc herniation might be affecting your nervous system.
Neurological and Orthopaedic Testing
To confirm that a herniated disc is the culprit irritating a nerve, we perform a series of specific tests. These are all non-invasive checks designed to see how well your nerves and musculoskeletal system are functioning.
You can expect procedures like these:
- Reflex Tests: Using a small reflex hammer on your knees and ankles to check how your nerve signals are responding.
- Muscle Strength Tests: Assessing the power in different muscle groups in your legs or arms. This helps us spot any weakness that might be caused by nerve compression.
- Sensation Checks: Lightly testing your ability to feel touch in different areas to map out any patches of numbness.
We also use orthopaedic tests, like the straight leg raise, which are designed to recreate the radiating pain in a controlled way. This helps us confirm exactly which nerve root is likely involved.
Deciding on Further Imaging
In most situations, a thorough physical examination gives us more than enough information to start a safe and effective course of care. However, if any "red flag" symptoms pop up or if your condition isn't improving as we'd expect, we might recommend further imaging.
An MRI (Magnetic Resonance Imaging) scan is usually the top choice here. It provides a crystal-clear picture of soft tissues, including the spinal discs and nerves, allowing us to see the exact location and size of the herniation. The decision to order an MRI is always made carefully to ensure it's truly necessary. The whole process is designed to leave no stone unturned, giving you confidence that your journey to recovery is starting with a complete and accurate diagnosis.
Building Long-Term Spine Resilience at Home
Getting lasting relief from a disc herniation is about more than just feeling better now—it’s about staying better for good. The hands-on treatment you get in the clinic is vital for that initial relief, but what really builds long-term resilience are the small, consistent choices you make every single day.
Think of this as your practical guide to transforming your daily habits and building a stronger, more robust spine right from home. The goal is to create an environment where your spine isn’t just surviving but actually thriving. This means being more mindful of your movements, strengthening the muscles that support your back, and tweaking your workspace to prevent re-injury.
Your Workspace and Daily Movements
Let’s be honest, many of us spend hours slumped at a desk, which puts relentless strain on the lower back if the setup isn’t right. An ergonomic workspace isn't a luxury; it's absolutely essential for your spinal health.
- Chair Height: Your feet should be flat on the floor, with your knees bent at a comfortable 90-degree angle.
- Screen Position: The top of your monitor should be at or just below eye level. This simple adjustment keeps your neck in a neutral, happy position.
- Lumbar Support: Use a small cushion or a chair with built-in support to help maintain the natural curve of your lower back.
Beyond the desk, how you lift things is critical. Always remember to bend at your knees and hips—never your waist. Keep the object close to your body and brace your core muscles. This simple technique protects your intervertebral discs from excessive, and often damaging, strain.
Exercises for a Stronger Core
Picture your core muscles as a natural corset that wraps around your midsection, giving your spine incredible stability. When these muscles are strong, they take a huge amount of pressure off your spinal discs. It’s no surprise, then, that targeted exercises are a cornerstone of preventing future flare-ups.
Gentle stretches and strengthening exercises not only improve flexibility but also build the muscular scaffolding needed for a healthy back. If you're looking for a deeper dive into specific movements, you can explore our guide on safe and effective exercises to strengthen your lower back.
Building a resilient spine isn't about gruelling workouts. It's about consistency and performing the right movements to create stability, which is your best defence against future disc problems.
Weaving these routines into your daily life helps lock in the progress you’ve made and fortifies your spine against the stresses of everyday activity.
To create lasting change, it helps to build small, repeatable actions into your day. Here are a few simple habits that can make a massive difference over time.
Simple Daily Habits for a Resilient Spine
Incorporate these actionable habits into your routine to support recovery and prevent future disc issues.
| Daily Habit | Why It Works | Quick Tip |
|---|---|---|
| Mindful Lifting | Protects discs from sudden, high-pressure loads that can cause re-injury. | Before you lift anything, pause and think: "Knees, not waist." Keep the object close. |
| 30-Minute Movement Break | Prevents muscle stiffness and disc compression from prolonged sitting. | Set a timer on your phone or computer. When it goes off, stand up, stretch, and walk around for 2 minutes. |
| Hydration Check | Intervertebral discs are mostly water; staying hydrated keeps them plump and shock-absorbent. | Keep a water bottle on your desk at all times. Aim to refill it at least 2-3 times during the workday. |
| Core Engagement | Activating your core muscles provides active support for your spine during everyday tasks. | When walking or standing, gently pull your belly button towards your spine, as if bracing for a light nudge. |
These small adjustments might not feel like much at first, but they compound over weeks and months, creating a much stronger and more resilient back.
For a broader perspective on building overall physical strength, which definitely contributes to long-term resilience, you might find this a practical guide to getting stronger helpful. By taking control of your daily habits and movements, you shift from being a passive recipient of care to an active participant in your own long-term well-being. This proactive approach is the real key to maintaining a pain-free, active lifestyle for years to come.
Of course. Here is the rewritten section, crafted to sound natural and human-written, following the provided style and requirements.
Your Questions Answered: What to Expect from Herniated Disc Care
It’s completely normal to have questions when you’re thinking about hands-on care for a herniated disc. In fact, it’s a good thing. Making smart decisions about your health is what this is all about, so let’s tackle some of the most common queries we hear. We want you to feel confident and clear about the road ahead.
Will the Treatment Hurt?
This is probably the number one question we get, and the short answer is no. Most people describe the treatments as feeling gentle and, most importantly, relieving. We use very precise, controlled techniques designed to be as comfortable as possible.
You might feel a bit of mild soreness afterwards—a bit like the feeling after you’ve worked a muscle you haven't used in a while—but sharp pain is definitely not part of the plan. We’ll be in constant communication during every session to make sure you’re comfortable. The whole point is to get you out of pain, not put you in it.
How Long Before I Feel a Difference?
Everyone’s recovery journey is a bit different, as it really depends on things like how severe the disc herniation is and your general health. That said, many patients tell us they feel a noticeable sense of relief from the worst of their symptoms within just the first few visits. That’s often because we’re starting to take the pressure off that irritated nerve straight away.
A full care plan, however, usually spans several weeks. This gives us the time not just to calm down the immediate pain, but to get to the root of the mechanical problem, strengthen the area, and stop it from coming back. We'll map out a realistic timeline for you at your first appointment.
Can This Help Me Avoid Surgery?
For a huge number of our patients, the answer is a big, resounding yes. Honestly, one of our main goals is to fix the problem without you ever needing to consider an invasive procedure like surgery.
There's solid clinical research showing that this kind of conservative care is very successful at reducing pain and getting people moving properly again. By doing this, it dramatically lowers the chances that someone will end up needing an operation for a lumbar disc herniation. Of course, there are rare or very severe cases where nerve function is seriously at risk, and in those situations, a surgical opinion is the right and necessary step.
Are you ready to stop managing the pain and start fixing the problem? The team at Spine, Body & Health is here to give you a clear diagnosis and a care plan that’s built just for you. Book your consultation online and take that first step towards getting your life back.




