Dealing with chronic back pain isn't just about managing the ache of the day; it's about breaking a frustrating cycle. To get lasting relief, you first have to understand why the pain keeps showing up, tackling the root causes like muscle imbalances and inflammation, not just the symptoms you feel on the surface.
Why Your Back Pain Keeps Coming Back
If you’re trying to figure out how to relieve chronic back pain, you’ve probably noticed it has a stubborn way of sticking around. It’s not like the sharp pain from a fresh injury that gets better with time. Chronic pain is a complex loop that can feel never-ending.
That’s because it’s rarely about one single event. It’s usually a collection of different factors that keep your body’s pain signals firing long after they should have stopped.
Getting to grips with this cycle is the first real step towards breaking it. Chronic back pain isn't just a physical feeling; it’s a multifaceted problem involving your muscles, your nerves, and even how your brain has learned to process discomfort.
The Cycle of Pain and Inflammation
When you first get injured, inflammation is a normal and healthy part of the healing process. But with chronic conditions, that response can get stuck on repeat.
Persistent inflammation irritates nerve endings, which then blast constant pain signals to your brain. Over time, your nervous system can become hypersensitive, meaning it starts to overreact to even the smallest movements or pressures.
This creates a vicious cycle: pain causes more inflammation, which in turn causes more pain. It explains why your back might feel okay one day and then be intensely sore the next, often without any obvious trigger.
The key takeaway here is that chronic pain often rewires how your body communicates with your brain. The goal isn't just to silence the pain but to interrupt the underlying cycle that keeps it active.
Common Triggers You Might Be Overlooking
So many of our daily habits unknowingly feed this cycle. A past injury might have been the starting point, but it's often our modern routines that stop us from ever fully recovering. Pinpointing these is essential for real, lasting relief.
- Prolonged Sitting: Spending hours slumped at a desk or behind the wheel can cause tight hip flexors and weak glute muscles. This imbalance forces your lower back to pick up the slack, leading to constant strain and fatigue.
- Poor Posture: Whether you’re hunched over your phone or always leaning to one side while standing, poor posture puts uneven pressure on your spine. Over time, this weakens the very muscles that are meant to support it.
- Subtle Muscle Imbalances: Sometimes, the problem isn't in your back at all, but in the muscles that are supposed to hold it up. A weak core, for example, fails to provide a stable foundation for your spine, leaving it vulnerable to strain. You can learn more about the specific causes of chronic back pain in our detailed guide.
This is a massive issue across the United Kingdom. Chronic back pain is a major health concern, affecting millions of people and standing as a leading cause of disability. In fact, statistics show that around 9.5 million people in the UK experience low back pain each year, which seriously impacts their quality of life and ability to work.
This just goes to show how vital it is to address the root causes early on to prevent long-term problems. You can discover more insights about the musculoskeletal health of the nation and its impact by reading the full report.
Building a Strong Foundation with Smart Movement
When you're living with constant discomfort, the thought of exercise can be intimidating, if not downright scary. But here’s something I’ve seen time and time again: gentle, consistent movement is one of the most powerful tools you have for managing chronic back pain. This isn't about pushing through agony with intense workouts. It's about intelligently rebuilding your body's natural support system from the ground up.
The aim is simple. We want to wake up and strengthen the muscles that are meant to support your spine, which takes a huge amount of strain off your lower back. When your core, hips, and back muscles start working together as a team, your spine no longer has to carry the entire load alone. It's a fundamental shift that leads to real, long-term relief.
Starting with Core Stability
Your core is so much more than your abs. Think of it as a natural corset, a complex group of muscles wrapping around your entire trunk to protect and stabilise your spine. After long periods of pain or sitting, these muscles often become weak or switch off, leaving your back vulnerable to strain from even the simplest daily activities.
A strong, stable core provides a solid base for every move you make, from walking down the street to lifting a bag of groceries. And you don't need punishing sit-ups to build it. The focus is on gentle, controlled exercises that activate those deep stabilising muscles.
- Pelvic Tilts: Lie on your back with your knees bent. Gently tighten your stomach muscles to flatten your lower back against the floor, then release. It’s a tiny movement, but it’s brilliant for waking up those deep core muscles without any strain.
- Bird-Dog: Get on your hands and knees. Slowly extend one arm straight out in front and the opposite leg straight back, keeping your back flat and your hips perfectly level. This challenges your balance and forces your core to fire up to keep you stable.
- Glute Bridges: Lie on your back, knees bent, feet flat on the floor. Squeeze your glutes and lift your hips until your body forms a straight line from your shoulders to your knees. This strengthens your glutes and hamstrings, which are vital partners in supporting the lower back.
The Importance of Flexibility and Mobility
Strength is only half the battle; flexibility is just as vital. Chronic pain often makes us stiffen up as the body tries to guard the sore area. Unfortunately, this creates a vicious cycle of more tension and less mobility. Gentle stretching is key to lengthening those tight muscles, improving circulation, and restoring a healthy range of motion.
The image below shows a gentle lumbar extension, a fantastic stretch for improving mobility in the lower back.
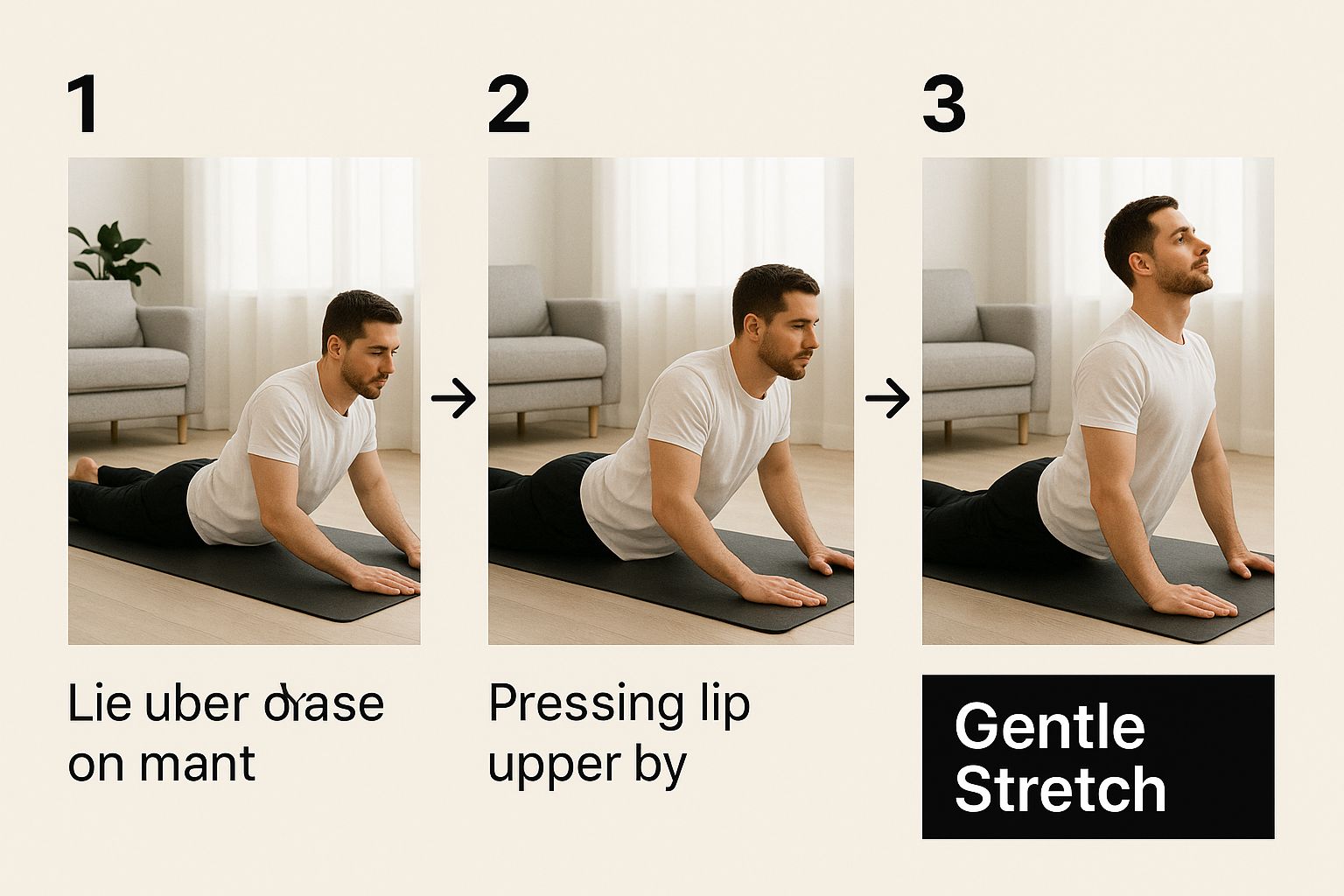
This simple, controlled movement is a great way to counteract the effects of sitting all day by gently extending the lower spine. For anyone looking for a more structured programme to regain strength and function at home, exploring in-home rehabilitation techniques can offer valuable, guided support.
Low-Impact Movement for Lasting Results
Let's be honest, high-impact activities are often a recipe for disaster when your back is already complaining. The good news? Low-impact exercises are incredibly effective for building strength and endurance without jarring your spine.
The key to smart movement is consistency over intensity. A short, daily walk or a 15-minute stretching routine performed regularly will deliver far more benefits than an occasional, strenuous workout that leaves you sore for days.
Weaving low-impact activities into your daily routine is a practical way to keep your body moving and your back supported.
Here is a simple routine you can start incorporating to build a healthier back. It's designed to be gentle but effective, helping you create a sustainable habit.
Daily Movement Routine for Back Health
| Movement Type | Focus Area | Frequency & Duration | Top Tip |
|---|---|---|---|
| Walking | Overall cardiovascular health and gentle spinal movement. | 20-30 minutes daily | Focus on standing tall and maintaining an upright posture; avoid slouching as you walk. |
| Swimming or Water Aerobics | Full-body conditioning with zero impact on joints. | 2-3 times per week, 30 minutes | The buoyancy of the water supports your body, allowing for pain-free movement. |
| Gentle Yoga or Pilates | Core strength, flexibility, and body awareness. | 2-3 times per week, 20-40 minutes | Look for beginner-level classes that prioritise slow, controlled movements. |
These activities don't just build strength; they also do wonders for your posture. If you want to tackle postural habits head-on, our dedicated guide on the best posture correction exercises is the perfect companion to your new routine.
By combining targeted strengthening, gentle stretching, and consistent low-impact movement, you can build a resilient foundation that protects your back from future flare-ups and helps you get back in control of your life.
Designing a Pain-Free Daily Environment

Your journey to relieve chronic back pain goes far beyond specific exercises; it extends right into the spaces where you spend most of your time. Your home and workplace can either be allies in your recovery or unknowingly contribute to your discomfort. With a few mindful adjustments, you can transform your environment into a supportive, pain-free zone.
The cumulative effect of poor ergonomics is huge. Hours spent slouched in a bad chair or sleeping on an unsupportive mattress place continuous, low-grade stress on your spine. This constant strain can undermine all your other efforts, making simple ergonomic changes one of the most effective strategies for long-term relief.
Optimising Your Workspace for Spine Health
For many of us, the workday involves hours spent sitting at a desk—a classic trigger for back pain. Creating an ergonomic setup isn’t complicated, but it does require paying attention to a few key details that make a world of difference. The goal is to support your spine’s natural curves, not force it into awkward positions.
Start by getting your chair right. Your feet should be flat on the floor with your knees at a 90-degree angle, roughly level with your hips. If your feet don't quite reach, a simple footrest will do the trick. Crucially, your lower back should be flush against the lumbar support of your chair to stop you from slouching forward.
Next, let's sort out your screen and keyboard.
- Monitor Height: The top of your computer screen should be at or just below eye level. This stops you from craning your neck up or hunching down, which puts immense strain on your upper back and neck.
- Keyboard and Mouse: Position your keyboard and mouse close enough that your elbows can stay comfortably by your sides, bent at about 90 degrees. Reaching too far forward causes your shoulders to round and your back to slump.
Remember, the best posture is your next posture. Even in a perfect setup, staying static is a problem. Set a reminder to get up, stretch, and walk around for a few minutes every half-hour to keep your muscles from seizing up.
The Critical Role of Restorative Sleep
Sleep is when your body does most of its healing and repair work, but an unsupportive mattress can turn this restorative period into eight hours of strain. If you regularly wake up feeling stiff and sore, your bed could be a primary culprit.
A mattress that's too soft lets your spine sag out of alignment, while one that's too firm can create painful pressure points on your hips and shoulders. Finding that sweet spot is key. A medium-firm mattress generally offers the best combination of support and comfort, but this is highly personal and depends on your sleeping position and body weight.
Our guide on how to choose the right mattress offers detailed advice to help you make an informed decision.
Mastering Everyday Movements
Often, a pain flare-up isn't triggered by a major event, but by a single, awkward movement during a routine task. Learning how to move mindfully can protect your back from unnecessary stress. Lifting is a perfect example of this.
Instead of bending over from your waist to pick something up—whether it's a laundry basket or a bag of groceries—always bend at your knees and hips. Keep your back straight, engage your core muscles, and use the power of your legs to do the lifting.
Hold the object close to your body to minimise leverage and strain on your lower back. This simple technique should become second nature for every lift, no matter how light the object seems.
Beyond the Basics with Advanced Therapies
So you've tweaked your daily movements and set up an ergonomic workspace, but that nagging back pain just won’t quit. When the foundational habits aren't cutting it, it might be time to bring in some more specialised support.
A number of evidence-based therapies can offer significant relief, working alongside your own efforts to get you moving freely again. These aren't just generic wellness tips; they’re targeted approaches designed to tackle the complex beast that is chronic pain. Many of these therapies work by interrupting the pain signals firing off to your brain or calming the deep-seated inflammation that simple remedies can't touch.
Think of them not as a replacement for smart movement and good posture, but as powerful additions to your recovery toolkit, especially when you feel like you've hit a wall.
Hands-On Manual Therapies
The core principle here is simple: good structure supports good function. When your spine, muscles, or joints are out of whack or restricted, pain is often the result. Skilled practitioners use hands-on techniques to get things moving properly again, release stubborn tension, and improve your body's overall mechanics.
Physiotherapy is often the first port of call, and for good reason. A good physio will assess your specific situation and create a personalised programme of exercises to strengthen weak areas and stretch out tight ones. They also use manual techniques to mobilise stiff joints and ease muscular tension, helping correct the imbalances that are feeding your pain.
Osteopathy offers a similar, yet distinct, perspective. An osteopath views the body as one interconnected system. Their goal is to improve its overall function by addressing restrictions in muscles, joints, and connective tissues. Using gentle manipulation, stretching, and massage, they work to boost blood flow, calm irritated nerves, and kick-start the body’s own healing processes.
Changing Your Relationship with Pain
Chronic pain isn't just a physical sensation—it has a huge psychological component. The relentless discomfort can trigger stress, anxiety, and a fear of movement, which then makes the pain feel even worse. It's a vicious cycle. Mind-body techniques are designed to break that loop by changing how your brain perceives and responds to pain.
Cognitive Behavioural Therapy (CBT): This approach helps you spot and reframe the negative thought patterns tied to your pain. Instead of thinking, "My back's gone, I can't do anything today," CBT teaches you to challenge that idea and find ways to adapt activities safely. It’s about giving you practical tools to manage flare-ups and reduce the emotional toll.
Mindfulness and Meditation: These practices train you to observe pain without judging it. Rather than tensing up in response, you learn to acknowledge the sensation and allow it to pass. In fact, studies show that regular mindfulness can decrease the perceived intensity of pain by up to 22%—fundamentally changing your experience of it.
Targeted Therapeutic Interventions
Beyond manual and mind-body work, several other therapies can offer targeted relief. These methods often zero in on specific pain pathways or sources of inflammation, adding another valuable layer to your recovery plan.
Acupuncture, for example, is a practice from traditional medicine where fine needles are placed at specific points on the body. This is thought to stimulate nerves and trigger the release of endorphins—your body’s natural painkillers. As you look into different therapies, it's helpful to understand the science behind them. You can discover the proven benefits of acupuncture for back pain to learn more about how it all works.
It's important to remember that these therapies are most effective when integrated into a broader management plan. They are not one-off fixes but part of a sustained effort to improve your back health from multiple angles.
There are also a few practical tools you can use at home to manage symptoms between appointments.
- Heat and Cold Therapy: Simple but effective. A heat pack can relax tight, aching muscles and improve blood flow. A cold pack, on the other hand, can help numb sharp pain and reduce fresh inflammation. Alternating between the two often works wonders.
- TENS Machines: A Transcutaneous Electrical Nerve Stimulation (TENS) device uses small electrical currents to disrupt pain signals. You place pads on the painful area, and the gentle pulses provide temporary but very welcome relief, making it easier to stay active.
Having an open conversation with your healthcare provider is the best way to figure out which of these therapies might be the right next step for you.
Adopting a Lifestyle for Lasting Back Health

True, lasting relief from chronic back pain is rarely a one-trick pony. All the exercises and therapies in the world can only get you so far. The real, sustainable solution is woven into the fabric of your daily life—your habits, the food you eat, and even how you manage stress.
Think of it as the final, crucial piece of the puzzle. By adopting a lifestyle that actively supports your spine, you’re not just managing pain; you're building a resilient, healthy back from the ground up. This approach gets to the root of what keeps the pain cycle going, tackling things like inflammation and chronic tension head-on.
Taming Inflammation Through Your Diet
You might be surprised how much the food on your plate affects the pain in your back. A diet heavy in processed foods, sugar, and unhealthy fats can pour fuel on the fire of inflammation, making chronic pain feel relentless and unpredictable. The good news is that the opposite is also true—an anti-inflammatory diet can help calm your system from the inside out.
Don't worry, you don't have to overhaul everything overnight. It's about making small, consistent swaps.
- Bring in the good stuff: Focus on whole foods packed with antioxidants and healthy fats. We’re talking leafy greens like spinach, colourful berries, nuts, and oily fish like salmon, which is loaded with omega-3s.
- Ease out the bad: Try to cut back on sugary drinks, refined carbs (white bread, pastries), fried foods, and processed meats. These are notorious for triggering an inflammatory response.
Every meal is a chance to either feed inflammation or fight it. It's an empowering way to take back some control over your pain.
The Connection Between Stress and Back Pain
Ever notice your back seems to ache more during a really stressful week at work? That's no coincidence. When you're stressed, your body pumps out hormones like cortisol that cause your muscles to clench up, especially around the neck, shoulders, and back. Over time, that constant tension turns into stiffness, soreness, and can even trigger a major flare-up.
This is a huge challenge for many people. In fact, over 22% of UK adults—that's more than 11.6 million people—live with chronic musculoskeletal pain. Back pain is often the main complaint, severely disrupting daily life. The socioeconomic impact is staggering, with cumulative lifetime costs for an individual sometimes exceeding £3.9 million from healthcare and lost earnings.
Making stress reduction a non-negotiable part of your routine is absolutely essential. To truly get a handle on chronic pain, it's worth looking into tools that address the mental and emotional side of things, too. You can also explore mindfulness as a pain management technique to build mental resilience against pain.
Managing stress isn’t a luxury; it’s a non-negotiable part of any effective plan to relieve chronic back pain. A calm mind often leads to a calmer, less painful body.
Foundational Habits for a Healthy Spine
Beyond what you eat and how you feel, a few other simple habits play a massive role in your back's long-term health. Think of these as the daily building blocks for a stronger, more supported spine.
Maintaining a Healthy Weight
Carrying extra weight, especially around your middle, pulls your centre of gravity forward. This puts constant strain on the muscles and ligaments in your lower back. The great news is that even a modest weight loss of 5-10% can dramatically reduce this mechanical stress and ease your pain.
The Importance of Hydration
The discs between your vertebrae are like little jelly-filled shock absorbers, and they're mostly made of water. When you're dehydrated, they can shrink and lose their cushioning ability, leaving you more vulnerable to pain and injury. Simply aiming for around two litres of water a day keeps these vital structures plump, healthy, and doing their job properly.
Got Questions About Chronic Back Pain?
When you’re trying to find your way out of chronic back pain, it’s natural to have a lot of questions. Let’s tackle some of the most common ones I hear from people, so you can move forward with a bit more clarity and confidence.
How Long Until I Feel Relief?
This is the big one, isn't it? The honest answer is: it’s different for everyone. Some people start to notice a real shift within a few weeks of sticking to targeted exercises and making simple ergonomic tweaks.
For others, especially if the pain has been a part of your life for years, it can take several months to feel significant, lasting relief. The most important thing to remember is consistency over intensity. Small, sustainable habits you do every day are far more powerful than going all-out once a week, which can often lead to a setback. Progress is rarely a straight line—expect good days and bad days along the way.
Here's a tip that really works: keep a simple journal. Note down your symptoms, how well you're moving, and just your general wellbeing. It's incredibly motivating to look back and see the gradual progress you're making, even when it doesn't feel like it day-to-day.
Patience really is your best friend on this journey. Aim for gradual improvement, not an overnight miracle. Celebrate the small wins, like sitting for ten minutes longer without that familiar ache or waking up with less stiffness. These are the true signs you're on the right track.
Focusing on the process and acknowledging these little victories creates a positive feedback loop. It encourages you to stick with your new routine, which is the absolute foundation for long-term recovery.
Is Bed Rest Good for a Sore Back?
For a very severe, fresh injury, your doctor might suggest a short rest period of 24-48 hours. But when it comes to chronic back pain, extended bed rest is almost always a bad idea. In fact, inactivity is one of the biggest hurdles to getting better.
When you stay still for too long, your muscles get stiff and weak. The deep core muscles that are meant to support your spine start to switch off, which can make the pain worse and drag out your recovery time.
Today, the consensus among professionals is all about gentle, active recovery. Movement is key. It helps reduce stiffness, gets blood flowing to the sore area to promote healing, and builds the strength your spine needs for proper support.
The guiding principle should be to "move with care"—don't avoid movement altogether.
When Should I See a Doctor?
While the strategies in this guide can make a huge difference, it is vital to see a GP or a qualified healthcare professional. This is especially true if your pain is severe, getting progressively worse, or if you notice any "red flag" symptoms.
You should seek immediate medical attention if you experience:
- Numbness, tingling, or weakness spreading into one or both of your legs.
- Any loss of bladder or bowel control.
- Unexplained weight loss, fever, or chills alongside the back pain.
Also, if your back pain started after a serious fall or accident, getting a proper medical diagnosis is essential to rule out anything serious. A professional assessment will give you a safe, personalised treatment plan that’s right for your specific situation. Think of this guide as a powerful tool for management, not a replacement for professional medical advice.
At Spine, Body & Health, we know just how complex chronic pain can be. Our focus is always on getting to the root cause, not just chasing symptoms. Since 2006, our team of dedicated practitioners in Milton Keynes has helped over 16,000 people find real, lasting relief. If you're ready to start your journey to a life with less pain, discover how our unique wellness care approach can help you.




