If you're looking for lasting relief from sacroiliac pain, the first step isn't just treating the symptoms—it's getting to grips with what’s actually happening deep inside your pelvis. Once you pinpoint the root cause, whether it's an old injury, overuse from your job, or a degenerative condition, you can finally move beyond simply masking the pain and start on a path to real, lasting relief.
Understanding Your Sacroiliac Joint Pain
Before you can fix the problem, you need to know what you’re dealing with. The sacroiliac (or SI) joint is a powerhouse. It's the critical connection point between your sacrum (that triangular bone at the very base of your spine) and your ilium, which is the big, wing-like part of your pelvic bone.
Think of it as the central hub absorbing all the shock and transferring force between your upper body, your pelvis, and down into your legs.
Now, unlike your shoulder or knee, the SI joint isn't built for big movements. Its main job is stability, allowing for just a tiny bit of give. When this joint gets inflamed, stiff, or isn't moving quite right, it leads to a condition we call SI joint dysfunction. This is an incredibly common source of nagging lower back, buttock, and sometimes even leg pain.
Common Causes Behind SI Joint Dysfunction
So, what throws this normally stable joint out of whack? Several factors can disrupt its function and lead to that familiar, persistent ache. Knowing what triggered yours is the key to managing it effectively.
- Traumatic Injury: A sudden jolt from a car accident, a hard fall, or even a sports injury can easily damage the strong ligaments supporting the SI joint. This can leave it feeling unstable or knocked out of its proper alignment.
- Repetitive Stress: It doesn't always have to be a big, sudden event. Activities that place repeated strain on the joint—like long-distance running or a physically demanding job that involves a lot of heavy lifting—can cause inflammation to build up slowly over time.
- Pregnancy and Childbirth: During pregnancy, the body releases hormones that cause ligaments to relax and loosen up to prepare for birth. While amazing, this increased flexibility can put a huge amount of extra stress on the SI joint, often leading to significant pain.
- Degenerative Conditions: Arthritis doesn't just affect knees and hips; it can settle into the sacroiliac joint, too. Ankylosing spondylitis, a type of inflammatory arthritis, frequently starts in the SI joints. Osteoarthritis can also cause the cartilage to wear down over time, leading to stiffness and pain. If this sounds familiar, you might find our guide on how it is possible to reverse osteoarthritis helpful.
The impact of spinal pain is significant, affecting not just physical comfort but overall quality of life. An effective management strategy is essential for anyone experiencing these symptoms.
Why This Pain Is So Prevalent
The burden of spinal pain is massive, and conditions like SI joint dysfunction are a huge part of the problem. A comprehensive study in Wales, UK, surveyed nearly 39,000 adults between 2016 and 2020 and found that around 4.95% were dealing with some form of spinal pain.
These UK spinal pain findings really highlight how widespread these issues are, making it crystal clear why finding effective management strategies is so crucial for improving people's well-being.
Gentle Movements For SI Joint Stability
When your sacroiliac joint is flaring up, the very idea of exercise can seem terrifying. I get it. But the right kind of movement is often the best thing for it. The goal isn't to push through pain, but to focus on gentle, controlled exercises that build stability around your pelvis and ease muscular tension. This creates a strong, supportive foundation that's key for long-term sacroiliac pain relief.
Think of it like this: small, everyday triggers—like lifting something awkwardly or sitting for too long—can slowly add stress to the SI joint until it finally protests.
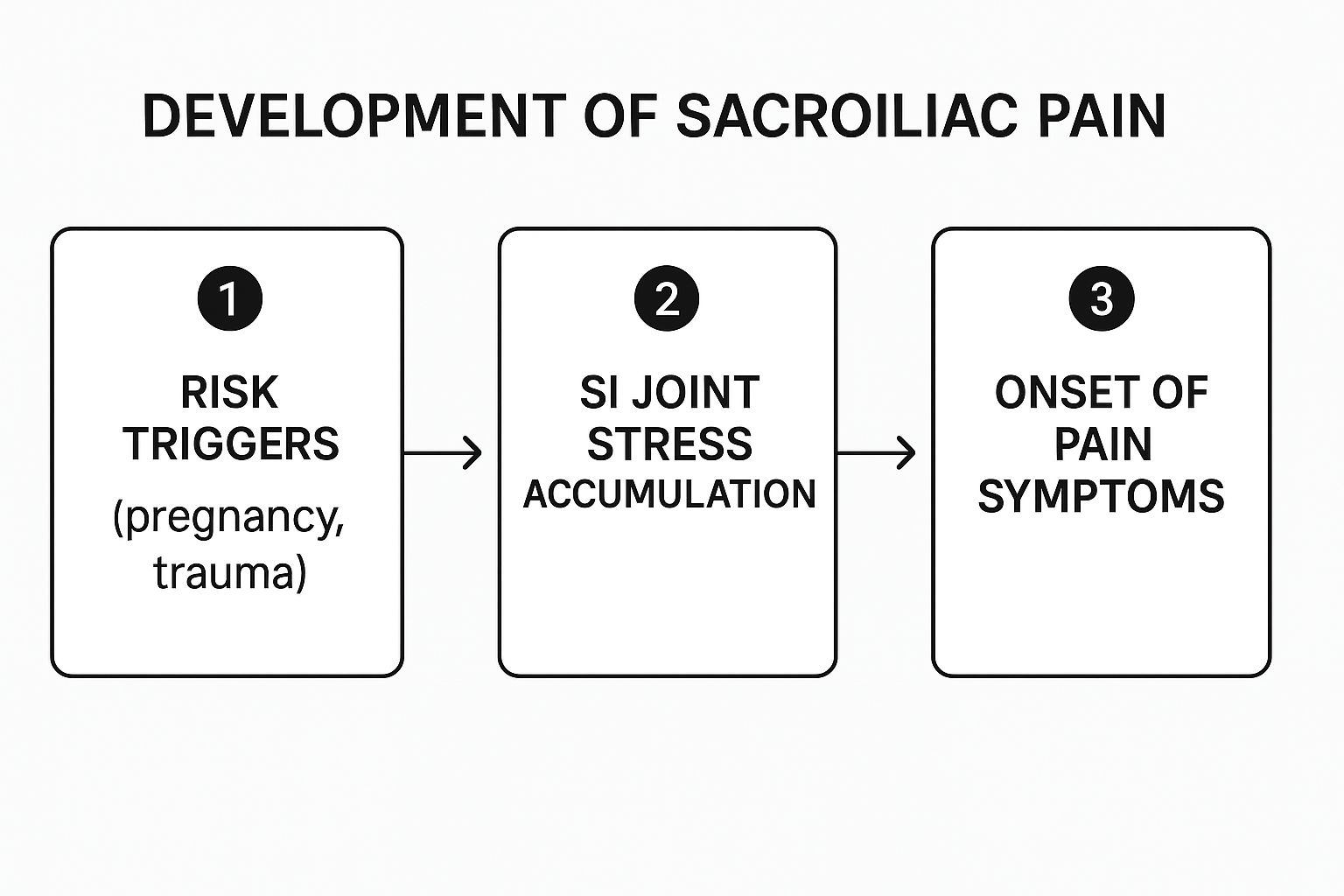
Understanding this build-up from trigger to pain is vital. Gentle movement helps interrupt that cycle by strengthening the very muscles that protect the joint from excessive strain in the first place.
Foundational Exercises For Pelvic Stability
Starting with low-impact routines is non-negotiable. These exercises are specifically designed to wake up the deep core and gluteal muscles—the ones that act like a natural corset for your pelvis, providing stability without causing more irritation.
Begin with these simple but surprisingly powerful movements:
- Glute Bridges: Lie on your back with your knees bent and feet flat on the floor. Gently lift your hips towards the ceiling, giving your glutes a good squeeze at the top. This move strengthens the primary muscles supporting the back of your pelvis.
- Knee-to-Chest Stretches: While still on your back, gently pull one knee towards your chest and hold it for 20-30 seconds. This is fantastic for releasing tightness in the lower back and glute muscles, which can often pull on the SI joint.
- Pelvic Tilts: Still lying down, gently flatten your lower back against the floor by engaging your core muscles, then release. It's a subtle movement, but it does wonders for improving your awareness and control over your pelvic position.
Many people also find that incorporating practices like exploring essential yoga poses for beginners can be a brilliant way to improve flexibility and core strength, which all contributes to lasting relief.
Common Exercises You Should Avoid
Just as important as knowing what to do is knowing what not to do. Certain common exercises can put way too much rotational or shearing force on the SI joint, which can easily make your pain worse. You'll want to be cautious with high-impact activities like running on hard surfaces or any intense twisting motions you might find in sports like golf or tennis.
It’s a common misconception that all lower back pain comes from the spine itself. In reality, the SI joint is a major player, and it’s often overlooked.
In fact, sacroiliac joint pain is a huge contributor to lower back issues here in the UK. Studies suggest it could be responsible for up to 25% of all cases of low back pain. That makes it an incredibly frequent, yet often missed, source of discomfort.
Because the symptoms can feel so similar, it's vital to figure out where your pain is actually coming from. If you're struggling to pinpoint the problem, our guide on understanding the main cause of lower back pain can offer some much-needed clarity. Ultimately, building a consistent, mindful movement practice is your best first line of defence in managing this specific type of pain.
A Daily Routine For SI Joint Support
Here is a sample schedule that integrates gentle exercises and posture habits to manage sacroiliac pain throughout the day.
| Time of Day | Activity | Purpose |
|---|---|---|
| Morning (7 AM) | Gentle Knee-to-Chest Stretches (in bed) | Loosen up the lower back and hips after a night of rest. |
| Mid-Morning (10 AM) | Stand and Walk Break | Prevent stiffness from prolonged sitting; encourage good posture. |
| Lunchtime (1 PM) | 5-Minute Pelvic Tilts | Re-engage core muscles and reset pelvic alignment. |
| Afternoon (3 PM) | 10 Glute Bridges | Activate glute muscles to support the pelvis during the afternoon slump. |
| Evening (8 PM) | Gentle Yoga or Light Stretching | Release the day's tension and improve overall flexibility before bed. |
Consistency is far more important than intensity. Even small, mindful movements spread throughout your day can make a significant difference in stabilising your SI joint and reducing your pain.
The gentle movements and exercises we've talked about are a brilliant foundation, but their benefits can be undone in a flash by habits you don't even realise you have. Your posture, the way you slump at your desk, even how you lug the shopping in from the car—it all plays a massive role in your sacroiliac pain relief journey.
Making small, mindful adjustments throughout your day is the key to reducing that constant strain on your SI joints.
So many of us spend hours sitting down without a second thought for how our posture is creating a pelvic imbalance. Slouching in a chair or leaning to one side places uneven pressure on your SI joints, gradually irritating them over time. The goal is to maintain a neutral pelvic position as much as possible, which often means consciously breaking those old, comfortable habits.
Fine-Tuning Your Everyday Ergonomics
Making a few simple ergonomic tweaks can bring profound relief by taking the stress off your pelvis. These aren't complicated, expensive fixes; they're practical changes that encourage your body's natural alignment.
Here are a few things you can try right away:
- At Your Desk: Sit with both feet flat on the floor, keeping your hips and knees at a rough 90-degree angle. A lumbar support cushion can be a complete game-changer here, as it helps maintain the natural curve of your lower back and stops your pelvis from tilting backwards.
- In Your Car: Adjust your seat so you aren't straining to reach the pedals or the steering wheel. Your knees should be level with or slightly below your hips. If you're on a long drive, a small rolled-up towel wedged behind your lower back can provide fantastic support.
- When Standing: Try not to lock your knees and make an effort to spread your weight evenly across both feet. If you have to stand for ages, shift your weight from side to side now and then, or pop one foot on a low stool to relieve the pressure.
Lifting Smarter, Not Harder
One of the most common triggers for an SI joint flare-up is lifting something the wrong way. It doesn't matter if it's groceries, a toddler, or a box from a delivery—your technique is everything. That classic advice to "lift with your legs, not your back" is especially critical for protecting your pelvis.
Always remember to bend at your knees and hips, keeping your back straight and pulling in your core muscles. Hold the object close to your body and, crucially, avoid twisting as you stand up. Twisting while lifting is a recipe for disaster when it comes to SI joint strain, as it puts a powerful shearing force right where you don't want it.
Your choice of footwear has a direct impact on the foundation of your pelvis. Shoes with zero arch support, like flimsy flip-flops or completely flat pumps, can throw off your gait and send shockwaves up through your legs straight into your SI joints.
Investing in a pair of supportive shoes with good cushioning is a simple but incredibly effective strategy. It helps absorb impact and promotes better alignment right from the ground up, giving your entire body a much more stable base to work with.
Understanding how these everyday choices affect your pelvic well-being is vital. For broader insights into maintaining general pelvic health and exploring natural approaches to pelvic discomfort, it's worth seeing how different issues can be connected. All these small changes add up, contributing to a more resilient and pain-free pelvic region.
Exploring Professional Therapies and Supports
When you’ve tried the gentle exercises and adjusted your daily habits but that nagging pain just won't budge, it might be time to bring in the professionals. Sometimes, self-care isn't enough to tackle the deep-seated muscle tightness and joint restrictions, and that's where hands-on therapies really shine.

Manual therapy from a trained professional, like a physiotherapist, is all about restoring proper movement and balance to your pelvis. They use specialised techniques to mobilise the SI joint, release tension in surrounding muscles like the glutes and piriformis, and correct any underlying alignment issues causing your discomfort.
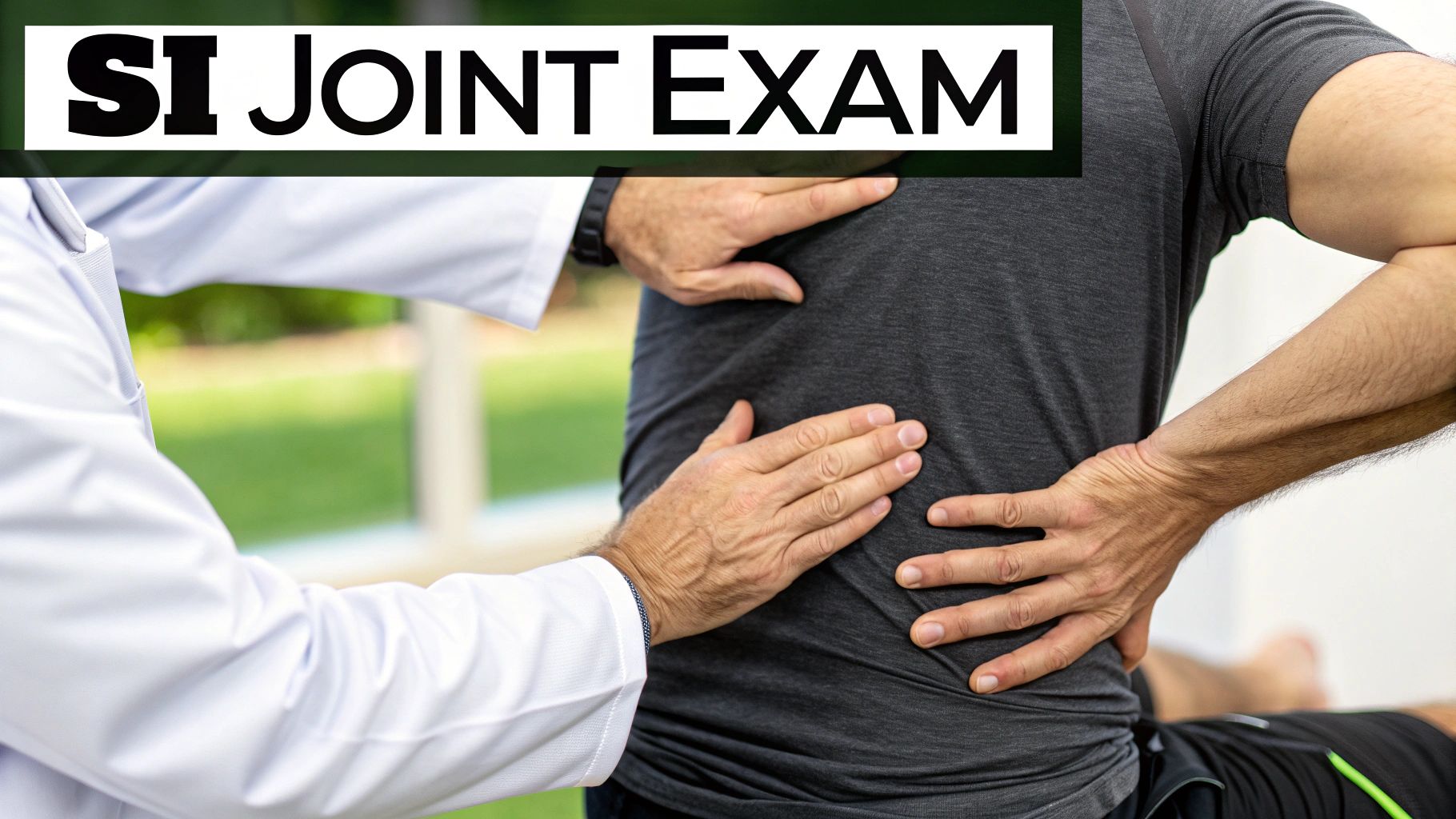
What To Expect From Hands-On Therapy
A good practitioner won't just start prodding you. They'll begin with a thorough assessment to understand your specific pain patterns and what's limiting your movement. This isn't just about chasing the symptom; it's about digging down to find the root cause.
Based on what they find, a typical treatment plan could involve:
- Soft Tissue Release: This means targeted massage and stretching to break up knots and tightness in the muscles around your pelvis and lower back. When these muscles are constantly tight, they can easily pull the SI joint out of its happy place.
- Joint Mobilisation: Here, your practitioner will use gentle, controlled movements to coax the SI joint back into its proper range of motion. It’s not about forceful cracking, but rather a subtle encouragement for the joint to move correctly again.
- Prescriptive Exercise: They'll also give you specific exercises tailored to your body's needs. The goal is to make sure you’re strengthening the right muscles to support your pelvic girdle for the long haul.
The Role Of SI Joint Belts And Supports
Alongside hands-on treatment, an SI joint belt can be a fantastic tool for immediate support and pain relief. It’s particularly helpful during activities that tend to trigger your symptoms. Think of it as giving your pelvis a supportive hug, mimicking the job of ligaments that might be strained or overstretched.
These belts are designed to be worn snugly around your hips, not your waist. When it’s in the right spot, the belt provides gentle compression that holds the SI joints together. This simple action can dramatically reduce those painful little micro-movements and help you feel more stable when you're walking, standing, or lifting.
An SI belt isn't a long-term cure, but a strategic tool. It's most effective when used during specific activities that cause flare-ups, such as gardening or long walks, rather than being worn all day.
Finding The Right Professional Support
Getting the right person in your corner is absolutely crucial for effective sacroiliac pain relief. You'll want to find a practitioner with specific experience in treating pelvic and lower back conditions.
A great professional will listen carefully to your history, perform a detailed physical examination, and create a personalised plan that combines hands-on work with an active home care programme.
Ultimately, professional therapies and supports act as a bridge. They give you the expert intervention needed to fix the immediate problem while empowering you with the tools and knowledge to manage your SI joint health on your own. This combination of professional guidance and personal effort is almost always the most successful route to lasting comfort.
Knowing When to Seek Medical Advice
While home care is a powerful first step in managing SI joint discomfort, it isn't always the complete solution. It's vital to know when to stop trying to fix it yourself and seek professional medical advice for your long-term sacroiliac pain relief. Certain signs are clear indicators that something more serious might be going on.

If your pain is severe, getting progressively worse despite your best efforts at home, or started after a significant injury like a fall or car accident, it’s time to get it checked. These are clear signals that your body needs a proper medical evaluation to figure out what's really happening.
Recognising Red Flag Symptoms
It's so important to listen closely to what your body is telling you. Some symptoms should never be ignored, as they may point to nerve involvement or other underlying issues that require immediate attention.
Keep an eye out for these warning signs:
- Numbness or Tingling: Any pins-and-needles sensation, numbness, or weakness spreading down into your legs or feet needs a professional look.
- Bowel or Bladder Changes: Any sudden difficulty with controlling your bladder or bowels is a medical emergency. Don't wait.
- Constant, Unrelenting Pain: Pain that just doesn't ease up, no matter if you rest or change positions, warrants a professional opinion.
- Fever or Illness: If your pain is accompanied by a fever or you just generally feel unwell, it could signal an infection that needs treating.
These symptoms go beyond what we'd expect from typical SI joint dysfunction and need a formal diagnosis to rule out anything more serious.
Understanding the diagnostic process can demystify the experience and help you feel more in control. It’s not just about finding pain, but about confirming its precise origin.
The Diagnostic Journey
When you see a specialist, they'll start with a detailed physical examination. This nearly always involves specific provocative manoeuvres where they gently stress the SI joint to see if it reproduces that familiar pain you've been feeling. While these tests are helpful, they’re just one piece of the puzzle.
Interestingly, imaging techniques like X-rays or MRIs often show limited value in diagnosing SI joint pain on their own. The real confirmation frequently comes from a more direct approach. A UK-based systematic evaluation found that the most reliable method is using controlled local anaesthetic blocks. In this procedure, an injection that provides 50% or more pain relief confirms the SI joint as the source.
Getting an accurate diagnosis is the most critical step toward finding the right treatment and getting lasting relief. If you're experiencing persistent symptoms and are unsure where to turn, finding a back pain specialist near me can set you on the path to an accurate diagnosis and a personalised care plan designed to bring you comfort.
Common Questions on Sacroiliac Pain Relief
As you start taking steps to tackle sacroiliac pain, it's natural for questions to pop up. You might be following a plan but wondering about the little details that can make a big difference. This section clears up some of the most common questions we hear, giving you that extra bit of confidence on your recovery journey.
Getting clear, straightforward answers helps you make smarter decisions about your daily habits and self-care, keeping you firmly on the path to feeling better.
How Long Does It Take to Find Relief from SI Joint Pain?
This is the big one, and the honest answer is: it really depends. The timeline for sacroiliac pain relief is tied directly to what's causing it in the first place and how consistently you're applying the right strategies.
If your pain is from a minor strain or a bit of temporary inflammation, you could feel a significant improvement within a few weeks of dedicated self-care. We’re talking about gentle exercises, posture adjustments, and just being more mindful of how you move.
However, for more chronic issues rooted in long-term instability or arthritis, relief is more of a gradual process. It can take several months of consistent effort to build up the muscle support your SI joints need and to calm down all that irritation. The key is to see it as a long-term management plan, not a quick fix. Progress isn't always a straight line—expect good days and bad days. That's a completely normal part of healing.
Can My Sleeping Position Affect Sacroiliac Pain?
Absolutely. You spend roughly a third of your life asleep, so your posture during those hours is critical. The wrong sleeping position can put prolonged stress on your SI joints, which is often why people wake up with that familiar stiffness and pain.
Your sleeping position has a profound impact on your pelvic alignment and can either help or hinder your progress. A single night in a poor position can undo a day of good habits.
Here’s how to set yourself up for better pelvic health overnight:
- Back Sleepers: This is often the best position. Try placing a pillow under your knees. This helps maintain the natural curve of your lower back and keeps your pelvis in a nice, neutral position.
- Side Sleepers: If you’re a side sleeper, slide a firm pillow between your knees. This is a game-changer because it stops your top leg from falling forward and twisting your pelvis, which is a common trigger for SI joint strain.
- Stomach Sleepers: We generally advise against this one. Sleeping on your stomach can flatten your spinal curve and throw your pelvis out of balance.
Should I Use Ice or Heat for SI Joint Pain?
It can be confusing trying to decide whether to grab an ice pack or a heating pad. They both have a place in your sacroiliac pain relief toolkit, but they do very different jobs.
Use ice for acute flare-ups or right after an activity that's made you sore. The cold helps to reduce inflammation and numb sharp pain. Just apply it for 15-20 minutes at a time.
Use heat—like a warm pack or a warm bath—for that chronic stiffness and general muscular ache. Heat is fantastic for relaxing tight muscles and improving blood flow to the area, which can help promote healing. Many people find that alternating between the two works best. The most important rule? Listen to your body and do what feels most soothing.
If you're tired of guessing and want a clear, personalised plan to address the root cause of your discomfort, the specialists at Spine, Body & Health are here to help. We are dedicated to providing effective solutions that bring lasting relief. Explore our approach and book your consultation at https://spinebodyhealth.co.uk.