When you’re looking for effective trapped nerve lower back treatment, the first step is to understand what’s actually going on. The goal is always to relieve pressure on the nerve and calm down the inflammation, and for most people, a sensible mix of rest, gentle movement, and professional care brings welcome relief from that sharp, nagging pain.
What a Trapped Nerve in Your Back Feels Like
Ever had a kink in a garden hose? The water can’t flow properly, causing pressure to build up and disrupting the whole system. That’s a brilliant way to picture what’s happening with a trapped nerve in your lower back. Your nerves are like the body’s electrical wiring, constantly firing signals between your brain and everywhere else. When one of those wires gets squeezed or compressed, the signals get scrambled.
This compression doesn’t just happen out of the blue; it’s a direct result of something happening in your lumbar spine—the lower part of your back. This area is a brilliantly complex structure of bones (vertebrae), cushioning discs, muscles, and ligaments, all working together to hold you up and let you move. But when a structure like a bulging disc or an overgrown bone spur pushes on a nerve root as it leaves the spine, you get that "kink," and the nerve can’t do its job properly.
The Anatomy of Nerve Pain
Your lumbar spine is made up of five large vertebrae. Tucked between each one is a soft, gel-like disc that acts as a shock absorber for every step you take. Nerves branch out from your spinal cord through small gaps between these vertebrae, heading down to your legs and feet.
When one of these nerves gets compressed, its ability to send clear signals is thrown into chaos. This disruption is what causes the classic symptoms you might be feeling.
- Pain Signals: Instead of normal messages, the squashed nerve sends out erratic, high-intensity pain signals. You might feel this as a sharp, shooting, or burning sensation.
- Sensory Disruption: The interference can also lead to strange sensations like tingling, "pins and needles," or even complete numbness in the area the nerve serves.
- Motor Command Issues: If the compression is bad enough, it can weaken the signals telling your muscles what to do, leading to noticeable muscle weakness in your leg or foot.
A trapped nerve isn't just a simple ache; it's a neurological problem. The pain you feel is your body's alarm system screaming that a critical communication line is under pressure and needs sorting out.
To give you a clearer picture, here is a quick summary of the most common signs you might be dealing with a trapped nerve in your lower back.
Quick Overview of Trapped Nerve Symptoms
| Symptom Type | Common Sensations |
|---|---|
| Pain | Sharp, shooting, burning, or aching pain that often travels from the back into the buttock, leg, or foot. |
| Altered Sensation | Numbness, tingling ("pins and needles"), or a "prickly" feeling in the affected leg or foot. |
| Muscle Weakness | Difficulty lifting the foot or toes (foot drop), or a general feeling of weakness or heaviness in the leg. |
| Positional Changes | Symptoms that get worse with certain activities like sitting, standing for a long time, coughing, or sneezing. |
This table helps break down the signals your body might be sending you. If any of these feel familiar, it's a good sign that something is irritating a nerve and a professional assessment can provide clarity.
How Common Is This Type of Pain?
If you're dealing with these symptoms, you are far from alone. Here in the UK, chronic nerve-related pain is a massive health issue. Research shows that neuropathic pain, which covers conditions like a trapped nerve in the lower back, affects a huge number of us. In fact, studies suggest that between 8% and 9.3% of UK adults are living with this kind of persistent pain, which really highlights why we need effective treatments. You can read more about these findings and what they mean for UK healthcare in this detailed study of neuropathic pain prevalence in the UK.
Understanding this foundation is the first real step toward finding a lasting trapped nerve lower back treatment. When you realise that the sensations are caused by physical pressure on a nerve, it’s easier to see how targeted therapies work to relieve that pressure and get things back to normal. This knowledge gives you the power to take the right steps on your road to recovery.
Why Nerves Get Trapped and How to Spot the Signs
To figure out the right treatment for a trapped nerve in your lower back, it helps to first understand why the nerve is under pressure in the first place. Think of your spinal nerves as busy motorways branching off the main spinal cord. For traffic to flow smoothly, these routes need to be clear. But sometimes, roadblocks pop up, causing a major traffic jam of nerve signals.
These roadblocks are the physical causes of nerve compression. They don't just appear overnight; they usually develop over time due to changes in the structures surrounding the nerves. Getting to know these common culprits is the first step toward clearing the path and finally getting some relief.
The Most Common Causes of Nerve Compression
Several conditions can narrow the spaces in your lower back and start to irritate a nerve. Each one creates pressure in a slightly different way, but the end result is the same: a nerve that can’t do its job properly.
This image shows some of the key reasons why nerves in the lower back become trapped, often linked to our daily habits and structural changes in the spine.
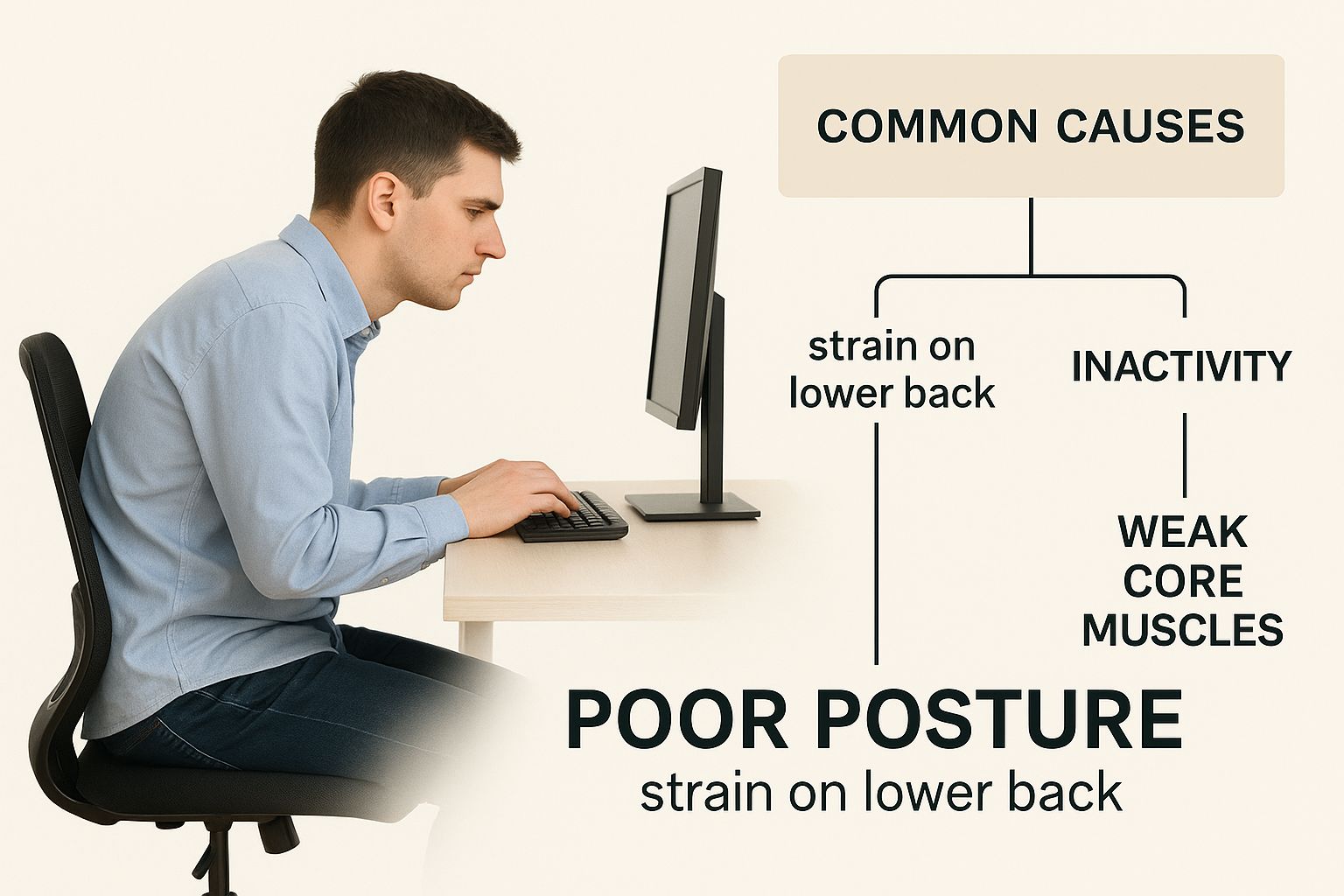
As the picture highlights, poor posture is a massive contributor. It places uneven strain on the spine over years, which can eventually lead to the structural problems that cause compression.
Let's break down the most frequent offenders:
- Herniated Disc: Many people call this a 'slipped disc', but that's not quite accurate. It's when the soft, gel-like centre of a spinal disc pushes out through a tear in its tougher exterior. This bulging material can press directly onto a nearby nerve root, triggering intense pain.
- Spinal Stenosis: This is essentially a narrowing of the spinal canal—the protective tunnel that houses your spinal cord and nerve roots. This narrowing can be caused by age-related changes like overgrown bone spurs (osteophytes) or thickened ligaments, which slowly squeeze the available space for the nerves.
- Degenerative Disc Disease: As we get older, our spinal discs naturally lose height and hydration. This can cause the vertebrae to sit closer together, narrowing the nerve passageways and sometimes leading to bone spurs that further irritate the nerves.
These conditions are incredibly common. Low back pain is a leading cause of disability here in the UK, and a huge number of cases involve some kind of nerve compression. One community study found that while 39% of adults had experienced low back pain in the last year, nearly 18% of them reported symptoms like referred pain or tingling that point directly to nerve trouble. You can read more about just how widespread this issue is by exploring the findings on low back pain prevalence.
How to Recognise the Warning Signs
Because a trapped nerve is a problem with your body's communication system, the symptoms feel very different from a simple muscle ache. They are neurological signals telling you that something is interfering with the nerve's pathway. Spotting these signs early is key to getting the right help.
You might experience a whole mix of symptoms that can range from mildly annoying to completely debilitating.
Recognising the type of sensation you're feeling is crucial. A sharp, electrical pain that travels is very different from a dull, localised ache and points more specifically to nerve irritation.
Here are the classic symptoms, broken down by what you might feel and notice.
Pain and Sensation Changes
The most well-known symptom is sciatica, that sharp, shooting pain that radiates from your lower back, through your buttock, and down the back of your leg. But the sensations can vary quite a bit:
- Burning or Aching Pain: A persistent, deep ache that settles in the buttock or leg.
- Tingling or "Pins and Needles": A fizzy, prickling feeling, which is technically known as paraesthesia.
- Numbness: A loss of sensation in parts of your leg, foot, or toes, which can feel really unsettling.
Muscle Function and Reflexes
When nerve signals to your muscles get disrupted, you might notice things aren't working as they should. These are important signs that you shouldn't ignore.
- Muscle Weakness: You may find it difficult to lift your foot (a condition known as foot drop) or feel that your leg "gives way" without warning.
- Loss of Reflexes: A clinician might notice reduced reflexes in your knee or ankle during an examination, which is a clear sign of a disruption in that nerve pathway.
Symptoms often get worse with certain activities like sitting for long periods, coughing, or sneezing. These actions can momentarily increase pressure on the compressed nerve, flaring things up. By connecting these specific signs to their underlying causes, you are far better equipped to have a productive conversation with a professional and move toward an effective treatment plan.
How Professionals Diagnose Your Nerve Pain
If you're stuck with persistent nerve pain, getting a professional diagnosis is the only real way forward to find a trapped nerve lower back treatment that actually works. It might feel a bit daunting, but understanding how we figure things out makes you a more confident partner in your own recovery. The goal is to stop guessing and get a crystal-clear picture of what’s truly causing your symptoms.
Any good clinician will start with a thorough chat about your medical history and the pain itself. They’ll want to know exactly what it feels like, where it travels, and what you do that makes it better or worse. This initial conversation gives us crucial clues that guide the entire examination.

The Physical Assessment
After we've talked it through, the next step is a hands-on physical assessment. This isn’t just a random series of tests; it's a systematic process to pinpoint which nerve is being affected and how badly it’s being squeezed. Think of it as a detective gathering evidence piece by piece.
Your practitioner will likely check a few key things:
- Reflexes: Tapping certain points on your knee and ankle is a quick way to check the health of your nerve pathways. A weak or absent reflex can point directly to compression at a specific level in your spine.
- Muscle Strength: We might ask you to push against our hand with your feet, ankles, or legs. Weakness in certain muscle groups is a classic sign telling us which nerve root is under pressure.
- Range of Motion: We'll assess how well you can bend and move your spine to identify any limitations and see which movements trigger your pain.
- Sensation Testing: The clinician may use a light touch or a small pinprick on different areas of your legs and feet to map out any numbness or changes in sensation.
These simple, non-invasive tests are incredibly powerful. They allow a professional to build a strong working diagnosis from clear physical signs, often without needing to jump straight to complex imaging.
Advanced Diagnostic Imaging
While a physical exam tells us most of the story, there are times when we need to take a look inside. This is particularly true if your symptoms are severe, aren’t getting better with initial treatment, or if there are any "red flag" signs we need to rule out.
Imaging is not always the first step. A good clinician uses these tools to confirm a diagnosis or plan a specific intervention, not as a substitute for a thorough physical exam.
Modern diagnostics are getting better all the time, using technology to get an incredibly precise view of the spine. For example, developments in AI for medical diagnosis are changing the game by helping professionals interpret complex scans with far greater accuracy.
The most common imaging tools we use include:
- Magnetic Resonance Imaging (MRI): This is the gold standard for looking at soft tissues. An MRI can clearly show a herniated disc, spinal stenosis, or inflammation pressing directly on a nerve.
- Computed Tomography (CT) Scan: A CT scan gives us excellent detail of the bones in your spine. It’s especially useful for spotting bone spurs or fractures that could be causing the nerve compression.
Understanding why and when these scans are needed helps demystify the process. If your practitioner recommends one, it’s to get the most accurate diagnosis possible. You can learn more about what these scans reveal in our detailed guide to nerve scans. This knowledge empowers you to ask the right questions and feel confident about the path forward to lasting relief.
Finding Relief at Home with Self-Care Strategies
When a trapped nerve in your lower back flares up, the first thing on your mind is getting some relief—and fast. While seeing a professional is key for a long-term fix, there are some really effective things you can do at home to manage the pain and kick-start the healing process. These first steps are all about calming that angry nerve and making sure you don’t aggravate it further.
The goal of any trapped nerve lower back treatment you try at home is to dial down the inflammation, ease up the muscle tension, and gently create a bit more space around the pinched nerve. You’d be surprised how much of a difference a few simple, consistent actions can make to your comfort levels, laying a solid foundation for your recovery.
The Right Way to Use Hot and Cold Therapy
One of the easiest first-aid tools you have is temperature therapy, but knowing whether to grab an ice pack or a hot water bottle is crucial. Get it wrong, and you could actually make things worse. It’s best to think of it as a two-stage approach for tackling inflammation and muscle tightness.
For the first 24 to 48 hours when the pain is at its sharpest, cold is your best friend. Popping an ice pack (wrapped in a thin towel) on the sore spot for 15-20 minutes at a time helps reduce inflammation and numbs those sharp pain signals. The cold constricts blood vessels, which limits the swelling around the nerve.
Once that initial intense, inflammatory phase has passed, you can switch over to heat for some soothing relief. A warm compress or a hot water bottle is brilliant for relaxing the tight, spasming muscles that almost always come with nerve pain. The warmth boosts blood flow to the area, bringing in fresh oxygen and nutrients to help it heal. It can be tricky to know which to choose, but our guide on using back pain heat or ice breaks it down clearly to help you get it right.
To make things simpler, here’s a quick comparison of what you can do at home.
At-Home Care Strategies At a Glance
| Technique | Primary Goal | How to Apply Safely |
|---|---|---|
| Cold Therapy | Reduce inflammation and numb acute pain | Apply an ice pack wrapped in a towel for 15-20 minutes at a time, especially in the first 48 hours. |
| Heat Therapy | Relax tight muscles and improve blood flow | After 48 hours, use a warm compress for 15-20 minutes to soothe muscle spasms and promote healing. |
| Gentle Stretching | Decompress the spine and improve mobility | Perform slow, controlled movements like the knee-to-chest stretch. Stop immediately if pain sharpens. |
| Posture Correction | Minimise daily strain on the lumbar spine | Use a lumbar roll when sitting, stand with even weight, and sleep on your back or side with pillow support. |
| Activity Modification | Avoid aggravating the nerve and allow healing | Identify and pause trigger activities (e.g., heavy lifting). Swap high-impact exercise for gentle walking. |
These strategies work together to create an environment where your body can start to heal itself, providing a crucial first line of defence against lower back nerve pain.
Gentle Stretches and Mobility Exercises
It might feel like the last thing you want to do when you're in pain, but complete bed rest is rarely the answer. In fact, gentle, controlled movement is vital for recovery. The secret is to perform stretches that decompress the lower back without putting any extra strain on that already irritated nerve.
Start with a few simple, safe exercises designed to ease the pressure:
- Knee-to-Chest Stretch: Lie on your back, knees bent. Gently bring one knee up towards your chest and hold it for 20-30 seconds. This gives the lower back muscles a nice, gentle stretch.
- Pelvic Tilts: Still on your back with your knees bent, gently press the small of your back into the floor by tightening your stomach muscles and tilting your pelvis up. Hold for a few seconds, then release.
- Cat-Cow Stretch: Get on your hands and knees. Slowly arch your back up towards the ceiling (like an angry cat), then gently let it sink down towards the floor (like a relaxed cow). This is great for promoting gentle movement in your spine.
Always listen to your body. If any movement causes that sharp, shooting pain down your leg to get worse, stop immediately. The goal here is gentle relief, not pushing through the pain.
The Power of Posture Adjustments
The way you hold yourself throughout the day plays a massive role in how much pressure your lower back is under. Making small, conscious tweaks to how you sit, stand, and sleep can bring about some serious relief.
- Sitting: Try not to slump. Sit with your back supported, feet flat on the floor, and your knees at roughly a 90-degree angle. A small rolled-up towel placed in the curve of your lower back can work wonders for maintaining its natural shape.
- Standing: Stand tall with your weight spread evenly across both feet. Avoid locking your knees and try to keep your shoulders back and relaxed.
- Sleeping: The best positions are usually on your back with a pillow tucked under your knees, or on your side with a pillow between your knees. This helps keep your spine in a neutral, happy alignment all night long.
Modifying Your Activities for Healing
Finally, it’s all about finding that sweet spot between rest and movement. Pushing through activities that clearly make your nerve pain flare up will only slow down the healing process.
This doesn't mean you have to stop moving altogether. It's more about being smart. Identify the specific movements or positions that trigger your symptoms—like sitting for too long or lifting something heavy—and take a break from them. You can swap high-impact exercises for gentler activities like walking or swimming, which keep you mobile without jarring your spine. Striking this balance helps your body heal properly without causing a setback, paving the way for a much quicker recovery.
Professional Therapies for Lasting Recovery
While home remedies are fantastic for calming a flare-up, getting lasting relief from a trapped nerve almost always needs professional guidance. Think of self-care as the first aid you apply right after an injury; professional therapy is the structured rehabilitation plan that rebuilds your strength and stops it from happening again. A targeted trapped nerve lower back treatment plan, designed by an expert, is your surest path to not only feeling better now but staying that way.
This professional approach goes far beyond simply chasing the pain. It’s all about digging deeper to find and fix the root cause of the nerve compression—whether that’s weak supporting muscles, stiff spinal joints, or ingrained movement habits that put your back under constant pressure. This is where a personalised programme truly shines, ensuring every exercise and adjustment is safe, effective, and perfectly matched to what your body needs.

Building a Stronger Back with Physiotherapy
A well-designed physiotherapy programme is usually the cornerstone of a successful recovery. It’s not just a sheet of generic exercises; it’s a dynamic, hands-on approach that combines manual techniques with specific movements to get you moving properly and without pain.
A huge part of this is manual therapy, where your practitioner uses skilled, hands-on techniques. This could involve gentle joint mobilisations to restore movement between your vertebrae, or soft tissue work to release those tight, spasming muscles that are squeezing the nerve. Getting your spine moving as it should is the first step to giving that irritated nerve the space it needs to calm down.
From there, you’ll be guided through a progressive exercise plan that typically includes:
- Core Strengthening Exercises: Building up the deep muscles in your abdomen and back creates a natural ‘corset’ that supports and stabilises your spine during everyday movements.
- Flexibility and Mobility Work: Gentle stretches for your hips and hamstrings are often included, as tightness in these areas can pull on the lower back and make things worse.
- Postural Re-education: Perhaps most importantly, you’ll learn how to sit, stand, and move in ways that protect your back, breaking the cycle of strain.
The real power of professional guidance is in the precision and safety it offers. An expert can make sure you're doing the exercises correctly, activating the right muscles, and not accidentally making that nerve irritation worse.
Specialised Techniques for Nerve Relief
Beyond general strengthening, practitioners often use specific techniques designed to work directly on the trapped nerve itself. One of the most effective is a set of movements called nerve gliding exercises—sometimes known as neural mobilisation or nerve flossing.
Imagine your nerve is like a piece of string running through a narrow tube. If it gets snagged or stuck, nerve gliding uses gentle, controlled movements to help it slide back and forth freely again. This simple action can help break down adhesions, improve blood flow to the nerve, and dial down its sensitivity. But technique is everything. Doing these exercises incorrectly can aggravate the nerve, which is another reason why expert supervision is so important.
The need for effective treatment is more pressing than ever. Over the last two decades in the UK, disability from low back pain has climbed, with studies revealing a 12% increase in the likelihood of it causing long-term problems. A huge number of these cases involve nerve root issues, leading to missed work and recurring pain. You can discover more about the growing impact of low back pain in the UK and see why getting early, effective help is so critical.
Ultimately, seeking professional help gives you a clear, structured roadmap to recovery. It combines an expert diagnosis with a personalised plan, empowering you with the tools and knowledge to build a stronger, more resilient back for the future.
Building a Stronger Back to Prevent Future Pain
Getting relief from nerve pain is a huge step forward, but the real win is making sure that pain stays gone for good. The final piece of the puzzle for any trapped nerve lower back treatment is building a stronger, more resilient back. This is all about making small, smart changes to your daily life to protect your spine long-term.
Think of it this way: your spine is the central support for everything you do. To keep it stable, you need to lighten its daily load while strengthening the muscles that hold it all together. It’s this proactive mindset that will be your best defence against another painful episode down the line.
Smart Ergonomics for Daily Life
So many of us spend hours slumped at a desk or standing in one spot, putting a huge amount of strain on the lower back without even realising it. A few simple ergonomic adjustments can make a world of difference.
- At Your Desk: Make sure your chair actually supports the natural curve in your lower back. Your feet should sit flat on the floor, and your screen needs to be at eye level to stop you from hunching forward.
- Around the House: When you're doing chores like washing up or ironing, try propping one foot up on a low stool. This little trick instantly takes the pressure off your lumbar spine.
These small tweaks add up, minimising the cumulative strain that often leads to nerve compression over time.
Master Proper Lifting Mechanics
One of the fastest ways to wind up back at square one is by lifting something the wrong way. The golden rule here is simple but crucial: always lift with your legs, not your back.
Keep the object you're lifting close to your body, bend at your knees (never your waist), and tighten your core muscles as you straighten up. This lets your powerful leg muscles do all the heavy work, shielding the delicate structures in your spine from harm.
Maintaining a healthy weight is another massive factor. Every extra pound you carry increases the load on your spinal discs and joints, which in turn raises your risk of nerve compression. Even losing a small amount of weight can significantly reduce this strain.
The Power of Consistent, Low-Impact Exercise
Regular movement is absolutely vital for a healthy spine. Low-impact activities are your best friend here—think walking, swimming, or cycling. They're fantastic because they boost blood flow and strengthen muscles without jarring your joints.
Remember, consistency beats intensity every time. Aim for 20-30 minutes of gentle activity on most days of the week to keep your back feeling healthy and flexible.
As you look to the long term, integrating fitness exercises that build core strength and stability is a powerful way to bulletproof your back. To get started on building that strong foundation, you can learn more about specific exercises to strengthen your lower back that help create a natural muscular 'corset' to support your spine.
By bringing these preventative habits into your daily routine, you’re not just avoiding pain—you’re taking back control of your spinal health and paving the way for a more active, pain-free life.
Your Questions Answered
When you're dealing with the sharp, nagging pain of a trapped nerve, it’s natural to have questions. Getting clear answers is the first step toward feeling in control and finding a path forward. Here are a few of the most common questions we hear.
How Long Does a Trapped Nerve Take to Heal?
This is usually the first thing people ask, and the honest answer is: it really depends. There's no single timeline that fits everyone.
For a minor case where the nerve is just a bit irritated, you might feel a real improvement in a few weeks with the right self-care and by adjusting your activities. But if the nerve is being more seriously compressed by something like a herniated disc or spinal stenosis, the road to recovery could be a few months long.
The healing speed comes down to what’s causing the problem, your general health, and how quickly you start an effective treatment plan. The most important factor? Consistency. Sticking with your exercises and therapies gives your body the best possible chance to heal properly.
When Should I Worry About My Nerve Pain?
Most of the time, nerve pain in the lower back can be managed with professional guidance and conservative care. However, there are a few "red flag" symptoms that you should never ignore. It’s vital to know when to stop trying to fix it yourself and seek urgent medical help.
Get in touch with a medical professional straight away if you experience any of these:
- Sudden, severe weakness in your leg or foot, like finding you can't lift your foot properly (this is known as 'foot drop').
- Loss of control over your bowel or bladder, or a strange numbness in the saddle area (your groin and inner thighs).
- Pain that is completely unrelenting and doesn't get better no matter what position you're in.
- The pain comes with a fever or unexplained weight loss.
These symptoms can point to a more serious condition that needs to be looked at immediately to prevent any risk of long-term damage. Don't second-guess it—seek emergency care if they show up.
Can a Trapped Nerve in the Back Heal on Its Own?
It's possible, but not something you should count on. A very mild bit of nerve irritation might settle down on its own, especially if it was caused by temporary inflammation that goes away with a bit of rest.
However, just waiting and hoping can be a risky game. The underlying mechanical problem—like a bulging disc or a narrowed spinal canal—rarely fixes itself. Without professional help to get to the root cause, the issue can linger, turn into a chronic problem, or keep flaring up again and again.
Getting a proper diagnosis and following a structured treatment plan is the most reliable way to ensure a full recovery. It also helps you build the strength and stability needed to stop the pain from coming back.
If you are tired of living with lower back pain and are looking for a lasting solution, the team at Spine, Body & Health is here to help. Our specialists focus on diagnosing the true cause of your pain to create a personalised recovery plan. Take the first step towards a pain-free life and find out more about our approach at https://spinebodyhealth.co.uk.