At its simplest, piriformis syndrome is a pressure problem. It happens when the piriformis, a small muscle tucked deep in your buttock, gets too friendly with the sciatic nerve running right beside it—compressing or irritating it.
Imagine a garden hose lying on a footpath. Most of the time, it’s fine. But if you accidentally place a heavy, knotted mat on top of it, the flow gets pinched off. Your sciatic nerve is the hose, and a tight, angry piriformis muscle is that mat.
Decoding Piriformis Syndrome
Piriformis syndrome is one of those incredibly frustrating conditions where a tiny, often-ignored muscle ends up causing a world of pain. This muscle, hidden deep within your glutes, is vital for rotating your hip and keeping you stable. The trouble starts when it becomes tight, goes into spasm, or gets swollen.
When that happens, it can directly interfere with the longest nerve in your entire body: the sciatic nerve.
This compression is the heart of the matter. The pain, tingling, and numbness it causes are often mistaken for sciatica that originates in the lower back, but the real source of the problem is muscular, not spinal. Understanding this distinction is the first, most crucial step toward getting the right help and finding lasting relief.
The Core of the Problem
When you strip it all back, piriformis syndrome is really just a mechanical conflict. You have a muscle and a nerve fighting for space in a very crowded neighbourhood. The main things that spark this conflict include:
- Muscle Tightness and Spasm: Overdoing it with activities like running or cycling can make the piriformis tighten up and spasm, squeezing the space available for the sciatic nerve.
- Prolonged Sitting: A sedentary lifestyle is a major trigger. Sitting for hours on hard surfaces or even with a wallet in your back pocket puts constant, direct pressure on the muscle.
- Direct Trauma: A nasty fall or an accident can cause inflammation and swelling in the buttock, directly impacting both the piriformis and the nerve next door.
- Anatomical Variations: For about 15% of people, the sciatic nerve actually passes through the piriformis muscle instead of underneath it. This anatomical quirk makes them far more likely to experience compression.
The key takeaway here is that the pain isn't random; it's a direct consequence of the piriformis muscle getting in the sciatic nerve's way. Figuring out which of these factors are at play for you is essential for creating a successful recovery plan.
To give you a clearer picture, here’s a quick breakdown of the main players involved in this condition.
Piriformis Syndrome at a Glance
| Component | Role in This Condition |
|---|---|
| Piriformis Muscle | A small, deep buttock muscle responsible for hip rotation. When it becomes tight, spasmed, or swollen, it is the primary source of nerve compression. |
| Sciatic Nerve | The longest and widest nerve in the body, running from the lower back down to the feet. Its proximity to the piriformis makes it vulnerable to irritation. |
| Gluteal Region | The buttock area where the muscle and nerve interact. This is where the mechanical conflict occurs and where symptoms often originate. |
| Hip Joint | The piriformis helps control this joint's movement. Imbalances or overuse related to hip function often contribute to the muscle becoming problematic. |
Understanding these components helps you see how interconnected everything is. The goal isn't just to treat the pain, but to understand why that little muscle is so unhappy in the first place.
Our aim is to dig into these causes in more detail, helping you connect the dots between your daily habits, your body’s unique mechanics, and the symptoms you’re feeling. Once you grasp the root cause, you can start taking informed, effective steps toward finally resolving the pain for good.
Your Body's Blueprint and Piriformis Pain

While daily habits and injuries are common culprits, sometimes the answer to "what causes piriformis syndrome?" is written into your body’s own unique blueprint. Your anatomy—specifically the relationship between your piriformis muscle and sciatic nerve—can set the stage for pain long before you feel the first twinge.
Deep within your glutes, these two structures have a very close working relationship. For most of us, the arrangement is straightforward: the sciatic nerve, a thick cable of nerve fibres, passes directly underneath the flat, pear-shaped piriformis muscle. It's a neat and tidy setup that usually allows both to do their jobs without getting in each other's way.
However, our bodies aren't all built from the same plans. In a significant number of people, nature has drawn a slightly different anatomical roadmap.
When Nerves Take a Detour
For some individuals, the sciatic nerve doesn't just pass cleanly beneath the muscle. Instead, it takes a more intimate route, creating a scenario where nerve compression is far more likely. This isn't a defect, but simply a natural anatomical variation that can make someone more prone to developing piriformis syndrome.
There are a few ways this can look:
- The Split Path: The most common variation is where the sciatic nerve divides into two branches before it even reaches the piriformis. One branch passes underneath as usual, but the other one pierces directly through the muscle fibres.
- The Direct Route: In less common cases, the entire sciatic nerve takes a shortcut right through the centre of the piriformis muscle.
- The High Road: Rarely, the nerve might pass over the top of the muscle instead of underneath it.
These variations are completely silent and cause no issues on their own. The trouble starts when the piriformis muscle becomes tight, inflamed, or goes into spasm.
Think of it like a thread passing through the middle of a sponge. When the sponge is relaxed, the thread can move freely. But if you squeeze that sponge, it directly constricts the thread, creating tension. This is precisely what happens when the sciatic nerve runs through the piriformis.
A Built-In Vulnerability
This structural difference explains why two people can do the same activity—like a long run or a day spent sitting at a desk—yet only one develops that nagging piriformis pain. The person with the anatomical variation has a built-in vulnerability. For them, even minor muscle tightness can lead to direct and immediate nerve compression.
This is backed by evidence showing that anatomical factors play a huge role in piriformis syndrome. In the UK, studies have found that around 16-17% of individuals have these kinds of anomalies where the sciatic nerve and piriformis muscle interact differently, predisposing them to nerve entrapment. You can explore more about these anatomical insights and their clinical implications. This is a critical piece of the puzzle, explaining why some people seem predisposed to this frustrating condition.
Everyday Habits That Trigger Piriformis Syndrome

While your unique anatomy might make you more prone to piriformis pain, it's often our everyday routines that light the fuse. The real answer to "what causes piriformis syndrome?" usually lies in the small, repetitive stresses we put our bodies through, day in and day out.
These triggers often fall into a few clear categories, which can help you connect the dots between your lifestyle and your pain. From the office chair to the running track, plenty of common activities can push the piriformis into a state of chronic irritation.
The Sedentary Strain
One of the most common culprits in our modern world is prolonged sitting. When you're sat for hours on end, especially on a hard surface or with poor posture, you’re putting direct, continuous pressure on the piriformis muscle. This constant compression restricts blood flow and, over time, can lead to tightness and inflammation.
It's the classic 'desk-job posture' effect. Slouching or leaning forward shifts your pelvis into a less-than-ideal position, which forces the piriformis to work overtime just to keep you stable. After weeks and months, this constant, low-level strain is often all it takes to trigger persistent pain and sciatic nerve irritation. Learning how to sit properly at your desk is a fundamental first step in taking this pressure off.
Overuse and Repetitive Motion
At the other end of the spectrum is simply asking too much of this small muscle. The piriformis isn't built for heavy, repetitive work, and activities involving repeated hip rotation can easily overwhelm it.
We see this frequently in scenarios like:
- Long-distance running: The relentless forward motion, particularly on unforgiving surfaces like pavement, can lead to fatigue and tightness in all the hip rotators.
- Cycling: That bent-over position, combined with the constant pedalling motion, places the piriformis under continuous strain.
- Intense squatting: Lifting heavy weights without proper form or without your main glute muscles firing correctly can force the piriformis to compensate, leading to a classic 'weekend warrior' type of strain.
In these cases, the muscle becomes overworked, resulting in inflammation and spasms that squeeze the nearby sciatic nerve.
Direct Trauma and Injury
Sometimes, the cause is far more sudden. A slip and fall directly onto your buttock, or the impact from a car accident, can cause immediate trauma to the gluteal region. This can lead to bleeding inside the muscle, significant swelling, and eventually, the formation of scar tissue.
This kind of acute injury creates an environment of inflammation and physical disruption. The resulting swelling and muscle guarding can directly impinge on the sciatic nerve, triggering the classic symptoms of piriformis syndrome almost instantly.
Even long after the initial injury seems to have healed, the scar tissue left behind can reduce the muscle's flexibility. This makes it much more prone to getting tight and irritated down the road. Understanding these triggers is key, as it allows you to connect your specific activities to the pain you're feeling and start making targeted changes for relief.
The Vicious Cycle of Muscle Spasm and Nerve Pain
When piriformis syndrome takes hold, it’s not just a case of a tight muscle. It quickly becomes a self-perpetuating cycle where pain and muscle tension feed off each other, creating a downward spiral that’s tough to break. Understanding this physiological loop is the first step to figuring out why the pain just won't go away and what it really takes to stop it.
It usually starts with an initial trigger, something as simple as overuse from a long run or the constant pressure from sitting at a desk all day. This initial stress causes microscopic damage or inflammation deep within the piriformis muscle. Your body's natural response is to guard the injured area, so the muscle clamps down in a protective spasm.
But this well-intentioned defence mechanism is where the real trouble begins.
How Spasm Fuels More Pain
A muscle stuck in a constant state of spasm can't function properly. This sustained clenching severely restricts blood flow to the area, which is a big problem. Less blood means less oxygen and fewer nutrients reaching the muscle tissue – the very things it needs to repair itself and stay healthy.
At the same time, this lack of circulation traps metabolic waste products, like lactic acid, within the muscle fibres. This build-up acts like a chemical irritant, further aggravating the muscle and, crucially, the sciatic nerve that runs right beside or through it. The nerve becomes increasingly sensitised, firing off more urgent pain signals to your brain.
Your brain interprets this escalating pain as a sign of a persistent threat. In response, it sends signals back down to the piriformis, telling it to tighten even more to protect the area. This locks you into a frustrating cycle: spasm causes irritation, irritation causes pain, and pain causes more spasm.
This infographic breaks down the typical process a professional follows to distinguish piriformis syndrome from other conditions and arrive at an accurate diagnosis.
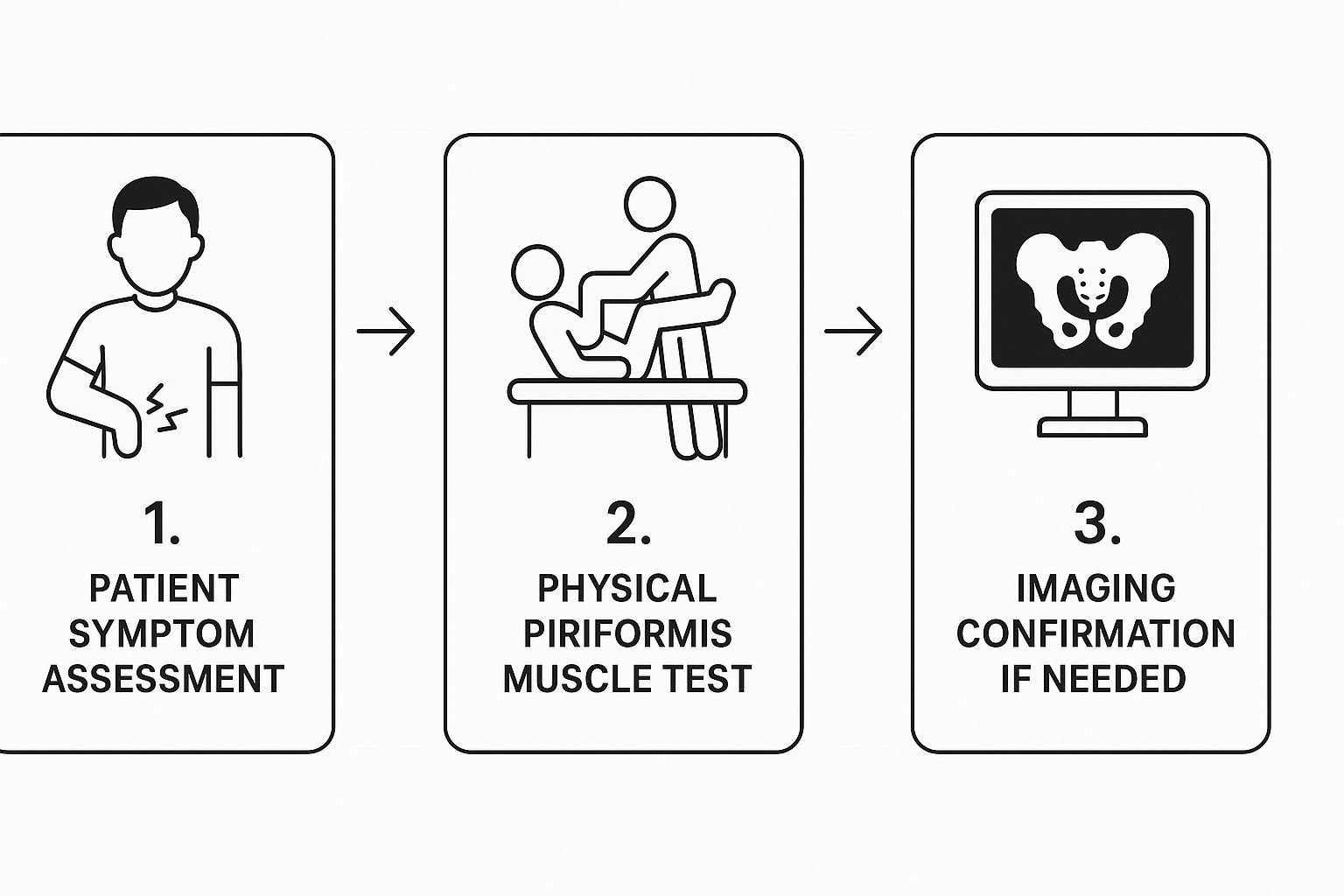
As you can see, a proper diagnosis is a methodical process. It always starts with listening carefully to your symptoms before moving on to any hands-on tests.
Breaking the Cycle Requires Action
This vicious cycle explains why simply resting often isn't enough to resolve piriformis syndrome. Sure, passive rest might temporarily calm the muscle down, but it doesn't address the underlying issues of poor circulation, waste build-up, and nerve irritation. As soon as you get back to your normal activities, the cycle can easily kick off again.
To properly tackle the root cause of piriformis syndrome, which almost always involves significant muscle tightness, exploring effective strategies for reducing muscle tension is a vital part of the solution. Breaking the cycle requires targeted interventions designed to:
- Release Muscle Spasm: Actively releasing the deep-seated tension in the piriformis muscle itself.
- Improve Blood Flow: Restoring healthy circulation to flush out all those irritants and deliver healing nutrients.
- Calm the Sciatic Nerve: Reducing the inflammation and direct pressure on the nerve to quieten down the pain signals.
By taking a proactive approach, you can interrupt this self-sustaining loop. This gives your body the chance it needs to heal properly, putting you firmly on the path to lasting relief from piriformis pain.
Is It Piriformis Syndrome or Something Else?
When you’re dealing with deep buttock pain that shoots down your leg, it's easy to jump to conclusions. But getting to the root of the problem is critical, because several different conditions can feel remarkably similar. Figuring out "what causes piriformis syndrome?" often means first ruling out other, more common culprits. This makes it a classic ‘diagnosis of exclusion’—a healthcare provider has to play detective, eliminating other suspects before zeroing in on the piriformis muscle.
This process is absolutely vital. Why? Because the treatment for a tight piriformis muscle is worlds away from the approach needed for a spinal issue. Two of the most common lookalikes are a lumbar disc herniation and sacroiliac (SI) joint dysfunction. While they can all cause that tell-tale sciatic-like pain, the mechanics behind them are completely different. Knowing a bit about these differences can help you have a much more informed conversation with your specialist.
Distinguishing Piriformis from Other Pain Sources
A lumbar disc herniation—what many people call a "slipped disc"—happens when one of the cushion-like discs in your lower back bulges out and presses directly on a spinal nerve root. This is a very different mechanism from the muscular compression we see in piriformis syndrome. A skilled practitioner can often tell the difference through specific physical tests and by listening carefully to how you describe your pain triggers. For instance, pain from a disc problem often gets worse when you bend forward, cough, or sneeze, while piriformis pain is notorious for flaring up after you’ve been sitting for a while.
Another common source of confusion is the SI joint. This joint connects your pelvis to the very bottom of your spine, and if it becomes inflamed or isn't moving correctly, it can refer pain into the buttock and down the leg, closely mimicking nerve irritation. The pain pattern can be so similar that it takes a hands-on, skilled examination to tell the two apart. If you're concerned that nerve compression is the real issue, you can find out more about what causes a trapped nerve in our detailed guide.
Piriformis syndrome is actually a relatively rare cause of sciatica and lower back pain. Research really highlights how uncommon it is. One UK review, for example, looked at nearly 1,300 patients with back pain and sciatica and found that fewer than 1% were identified as having piriformis syndrome. You can learn more about the diagnostic challenges and prevalence of this condition and see why a thorough, expert examination is so important.
Symptom Comparison Table
To help clear things up, this table contrasts the typical signs of these three common conditions. Just remember, symptoms can and do overlap, which is exactly why a professional assessment is always the best way to get an accurate diagnosis.
| Feature | Piriformis Syndrome | Lumbar Disc Herniation | Sacroiliac (SI) Joint Dysfunction |
|---|---|---|---|
| Primary Pain Location | Deep in the buttock, often a specific tender point. | Lower back, radiating down one leg. | Lower back and buttock, often one-sided. |
| Pain with Sitting | Typically gets worse, especially on hard surfaces. | Can be better or worse, depending on posture. | Often worsens, especially when rising from a seated position. |
| Pain with Bending | Usually does not increase pain. | Often significantly worsens when bending forward. | Can be painful, but not as consistently as a disc issue. |
| Neurological Signs | Tingling/numbness is common, but muscle weakness is rare. | May include significant foot or leg weakness. | Less likely to cause distinct neurological symptoms. |
Finding Your Path to Lasting Relief
Understanding what causes piriformis syndrome is the essential first step toward recovery. As we've seen, it's often a complex puzzle of factors—your unique anatomy, daily habits like prolonged sitting, or even an old injury—that can lead to this painful condition. Connecting these dots is key, but the single most important thing you can do right now is get an accurate diagnosis from a qualified professional.
Self-diagnosing is a risky game that can easily lead to the wrong treatment and drag out your discomfort. We strongly encourage you to book an assessment to pinpoint the precise source of your symptoms. Taking this proactive step allows a specialist to build a recovery plan specifically for your body and lifestyle, which might include improving hip stability by learning how to strengthen your core muscles.
Taking control starts with a clear diagnosis. A personalised plan is the most effective route to moving beyond the pain cycle and achieving long-term relief from piriformis syndrome.
The financial burden of this condition is also growing, with UK treatment costs estimated to be around £6.1 million in 2024. This figure reflects a rising awareness of the condition, which only underscores the need for effective, professional care. For those exploring complementary therapies alongside professional guidance, you might find benefit in looking into natural pain relief solutions like castor oil.
Ultimately, a professional assessment is your best path forward. It ensures you receive the correct guidance to finally become pain-free and get back to living your life.
Your Questions, Answered
When you're trying to get to the bottom of what’s causing your piriformis pain, a lot of questions can come up. Here are some clear, straightforward answers to the ones we hear most often.
Can Bad Posture Cause Piriformis Syndrome?
Yes, absolutely. Poor posture, especially while sitting, is a huge contributing factor. When you slouch or lean to one side for hours on end, you create muscle imbalances around your pelvis. This forces the piriformis to work overtime trying to keep things stable, leading to tightness, fatigue, and eventually, that dreaded nerve irritation.
Think about it this way: habits like sitting with a wallet or phone in your back pocket put direct, constant pressure right on the muscle. Over time, this compression is more than enough to trigger the symptoms of piriformis syndrome.
Is This Condition More Common in Men or Women?
While piriformis syndrome can affect anyone, studies suggest it’s diagnosed more often in women. The exact reasons are still being explored, but it likely comes down to a mix of anatomical and biomechanical differences.
A woman's pelvis is naturally wider, which changes the angle and mechanics of the hip muscles. This can place the piriformis muscle under different lines of stress compared to a man's, potentially making it more susceptible to strain and tightness.
Will Piriformis Syndrome Go Away on Its Own?
For a very mild case caused by a simple, one-off strain, the pain might ease up if you rest and avoid whatever aggravated it. But honestly, that’s rarely a permanent fix.
If the real problem is a chronic muscle imbalance, poor movement patterns, or an anatomical issue, the pain will almost certainly stick around or come back without proper intervention. Lasting relief usually means getting to the root cause with targeted stretching, strengthening exercises, and professional guidance. Just resting doesn't correct the biomechanical habits that got you here in the first place.
Does Running on Pavement Cause Piriformis Syndrome?
Running on hard surfaces like pavement definitely increases the impact forces that travel up through your legs and into your pelvis. This repetitive stress can certainly contribute to piriformis irritation, especially if you already have weak glute muscles or less-than-perfect running form.
So, while the hard surface isn't the only cause, it can be a major aggravating factor that shines a spotlight on an underlying weakness in your body's mechanics.
At Spine, Body & Health, our specialists focus on uncovering the precise cause of your pain to create a lasting solution. If you are struggling with buttock or leg pain, don't wait for it to worsen. Book an assessment with our specialists in Milton Keynes today and take the first step towards a pain-free life.




