Ever felt a strange, nagging ache in a part of your body that makes no sense? Maybe a dull throb in your shoulder for no reason at all? This is often someone's first puzzling encounter with referred pain.
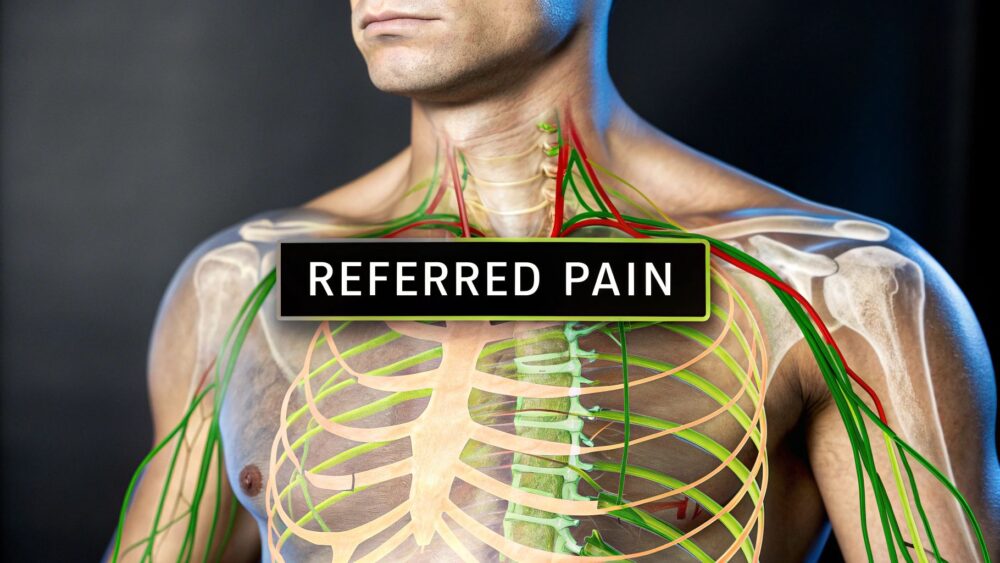
It’s a bizarre sensation where you feel discomfort in one area, but the actual problem is lurking somewhere else entirely. Think of it as a glitch in your body's wiring—a problem in an internal organ can trigger an ache in a muscle or joint that seems completely unrelated.
Decoding Your Body's Mixed Signals
So, how does this happen? Referred pain occurs because the nerves from different parts of your body—like your skin, muscles, and internal organs—often share the same pathways to the brain. Your brain is used to getting pain signals from muscles and skin, so when a signal comes from a less-talked-to internal organ, it can easily get its wires crossed.
It defaults to interpreting the signal as coming from a more familiar source, leading you to feel that confusing pain in an area that's perfectly healthy.

Distinguishing Referred Pain from Other Sensations
Pain isn't a one-size-fits-all experience. To really get to the bottom of what you're feeling, it helps to understand how referred pain stacks up against other types. Each has its own character and points to different root causes.
To make this clearer, here’s a quick rundown of the main types of pain you might experience.
Understanding Different Types of Pain
| Pain Type | What It Feels Like | Classic Example |
|---|---|---|
| Local Pain | Straightforward pain you feel right at the site of an injury. | A sharp sting from a paper cut or the throbbing from a stubbed toe. |
| Radiating Pain | Pain that starts in one place and travels along a nerve's path. | The sharp, shooting pain of sciatica running from the lower back down the leg. |
| Referred Pain | A deep, aching, and often hard-to-pinpoint ache in a healthy area. | Feeling pain in the left arm during a heart attack. |
Getting a handle on these distinctions is crucial, especially when you consider how common complex pain patterns are.
Chronic pain, which often involves referred pain, is incredibly widespread. In the UK, it affects an estimated 43% of the population. This highlights just how frequently conditions with confusing pain signals occur. Musculoskeletal issues like back pain are notorious for presenting with referred pain, which is why getting an accurate diagnosis is so important. You can dig deeper into the numbers by exploring a meta-analysis of chronic pain prevalence.
Here's a helpful way to picture it: imagine your body’s nervous system is a complex electrical grid. A short circuit in the kitchen (an internal organ) could surprisingly cause a light to flicker in the bedroom (your shoulder).
By understanding what referred pain is, you can start making sense of these confusing signals from your body. Recognising these patterns is the very first step towards getting the right help and uncovering the true source of your discomfort. The goal, after all, isn't just to chase the symptom—it's to fix the root cause.
How Your Body's Wiring Can Get Crossed
To really get your head around referred pain, you have to appreciate your body’s incredibly complex communication system. Think of your nervous system as a highly organised, but unbelievably busy, postal service. Every single second, millions of sensory messages are fired off from your skin, muscles, and internal organs, all addressed to your brain.
Your spinal cord is the main sorting office for all these messages. It’s in this central hub that nerve pathways from different parts of the body meet up and bundle together before making the final trip to the brain to be interpreted. It’s an efficient setup, for the most part, but it's not perfect. This is where the wires can get crossed.
The Brain's Educated Guess
Your brain is a master of pattern recognition. Over your lifetime, it has become an expert at reading signals from your skin and muscles. When you touch something hot or pull a muscle, the message is crystal clear, familiar, and easy for your brain to pinpoint.
But here’s the thing: your brain gets far fewer distress signals from internal organs like your heart, liver, or gallbladder. These organs don't have their own dedicated, high-priority nerve lines straight to the brain. Instead, their signals often have to hitch a ride along the same shared pathways used by nerves from more familiar locations.
This shared circuitry is the key to understanding referred pain. When a signal from a troubled organ arrives at the spinal cord, it merges into a pathway that also carries information from a specific patch of skin or muscle. The brain, receiving this muddled message, defaults to what it knows best. It makes an educated guess and blames the pain on the more common source—the muscle or skin—rather than the organ it rarely hears from.
Neural Convergence in Action
This whole process is known as neural convergence. It’s not a mistake or a malfunction, but simply a consequence of how our nervous systems are wired for efficiency.
Let's break it down step-by-step:
- Source of the Problem: An internal organ (like your diaphragm) gets irritated or injured.
- The Signal: It sends a pain signal through its sensory nerve fibres, heading for the spinal cord.
- The Crossroads: At a specific point in the spinal cord, these nerve fibres converge with nerves coming from a completely different body part (like your shoulder).
- The Brain's Interpretation: Both signals travel up to the brain together on the same track. Because the brain is far more used to getting signals from the shoulder, it interprets the pain as coming from there.
This concept map shows how the signal travels from the true source, through shared nerve pathways, to the site where you actually feel the pain.
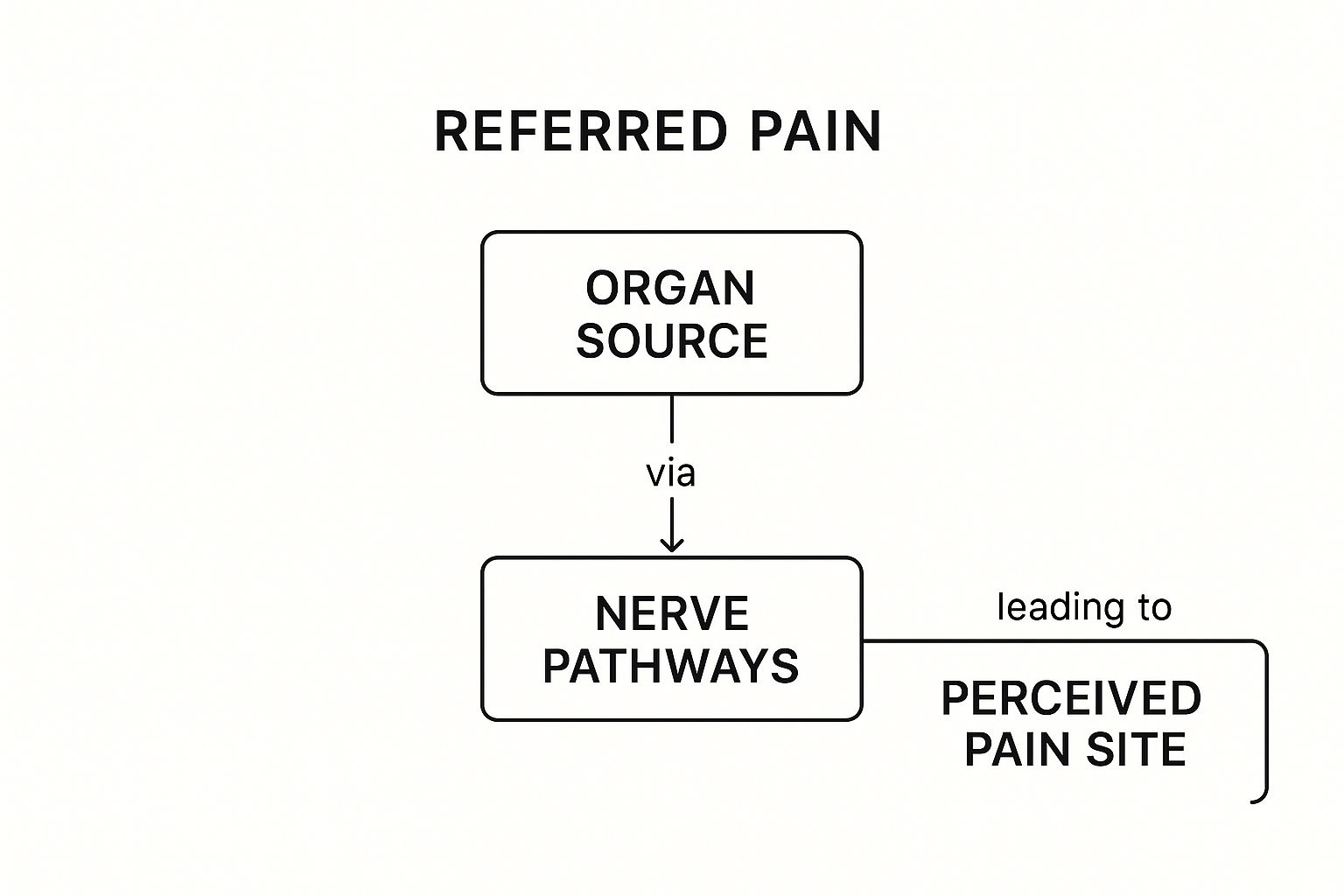
As the image makes clear, the place you feel pain can be a long way from the actual site of the issue, which highlights the diagnostic challenge it presents for both patients and practitioners.
Why This Signal Mix-Up Matters
This wiring quirk has some pretty significant real-world implications. A classic example is the shoulder pain that can pop up due to irritation of the diaphragm, the big muscle sitting just below your lungs. The nerves that supply the diaphragm (the phrenic nerve) actually start in your neck, at the very same level as the nerves supplying the skin and muscles of your shoulder.
As a result, when the diaphragm is irritated—perhaps by a problem with the liver or gallbladder sitting nearby—the brain misinterprets these signals and creates the sensation of pain in the shoulder.
This isn't just limited to organs, either. Musculoskeletal issues can create referred pain too. A problem in a spinal joint in your lower back can send a deep, dull ache into your buttock or down your leg, even without directly pinching a nerve. It's simply the brain misreading the source of the signals coming from that shared spinal level.
Understanding this mechanism is the first step toward decoding your body's confusing messages. The pain you feel is absolutely real, but its location can be a very misleading clue. Tracing that signal back to its true origin is essential for an effective diagnosis and, ultimately, for lasting relief. Without addressing the source, you're only ever treating a symptom of a deeper issue.
Common Patterns of Referred Pain
Knowing the theory behind referred pain is one thing, but recognising it in your own body is a completely different ball game. Now that we’ve touched on how the nervous system’s wires can get crossed, let’s look at some of the most classic patterns we see. These real-world examples are perfect illustrations of how a problem in one spot can shout for attention in a totally different, sometimes distant, part of the body.
Many of these patterns are so well-known they act as vital clues for healthcare professionals. Spotting them can help you make sense of confusing symptoms and understand why we always need to look at the bigger picture. It’s not just about what hurts; it’s about figuring out where that pain is really coming from.

Pain from Internal Organs
Some of the most dramatic examples of referred pain come from our internal organs. Think about it: your brain rarely gets direct messages from these structures, so when it receives an urgent signal, it often gets confused. It defaults to blaming a more familiar area—like a muscle or joint—that happens to share the same nerve hotline to the spinal cord.
Here are a few classic examples:
- Heart Issues and Left Arm Pain: This is probably the most famous one. Sensory nerves from the heart connect to the same part of the spinal cord (T1-T5) as nerves from the chest, left shoulder, and inner arm. During a heart attack, the brain gets this intense, unfamiliar signal and misinterprets it as coming from the arm. This biological mix-up has served as a critical warning sign that has saved countless lives.
- Gallbladder Problems and Right Shoulder Pain: This one’s a bit of a journey. The gallbladder sits right under the diaphragm, which is controlled by the phrenic nerve. This nerve originates high up in the neck (C3-C5). When the gallbladder gets inflamed, it irritates the diaphragm, sending a distress signal up the phrenic nerve. The brain traces it back to its source in the neck and concludes the problem must be in the right shoulder, which is supplied by nerves from the same area.
- Kidney Issues and Flank Pain: Pain from the kidneys often shows up as a deep, nagging ache in your side, in the area between your ribs and hips (the flank). This is because the nerves servicing the kidneys share pathways with those that supply the skin and muscles of the lower back.
Musculoskeletal Sources of Referred Pain
It’s a common myth that referred pain only comes from organs. In reality, muscles, ligaments, and joints are huge culprits. A problem in one of these structures can easily send pain elsewhere, leading to a whole lot of diagnostic confusion.
Take trigger points, for example. These are essentially tight, irritable knots of muscle that are notorious for referring pain. A small trigger point in the gluteus minimus muscle (deep in your buttock) can shoot a sharp, aching pain right down the back of your leg, perfectly mimicking sciatica. The source, however, isn’t a trapped nerve in your spine at all; it’s a dysfunctional muscle.
Referred pain from musculoskeletal sources often feels deep, achy, and is frustratingly difficult to pinpoint. You might find that pressing on the actual source of the problem—like a knot in your shoulder muscle—perfectly recreates the pain you feel in a seemingly unrelated area, like your head or down your arm.
This highlights a crucial point we always come back to: the location of your pain is not always the location of your problem.
To help you connect the dots, here’s a quick-reference table linking common pain locations to their possible origins. It’s a great way to start spotting potential connections yourself.
Common Referred Pain Patterns and Their Potential Sources
| Where You Feel the Pain | Where the Problem Might Be (The Source) | Associated Nerve Pathways |
|---|---|---|
| Left Arm & Jaw | Heart | Thoracic Nerves (T1-T5) |
| Right Shoulder Tip | Gallbladder, Liver | Phrenic Nerve (C3-C5) |
| Upper Back (between shoulder blades) | Stomach, Gallbladder, Pancreas | Thoracic Nerves (T5-T9) |
| Lower Back & Flank | Kidneys | Subcostal Nerve (T12) |
| Buttock & Back of Thigh | Sacroiliac (SI) Joint, Lumbar Facet Joints, Gluteal Muscles | Lumbosacral Nerves (L4-S3) |
Remember, this table is just a guide. A thorough diagnosis is essential to pinpoint the true cause of your discomfort accurately.
The Complexity of Leg Pain
Pain that travels down the leg is a perfect case study in just how tricky referred pain can be. Many people hear "leg pain" and immediately jump to sciatica, which is specifically pain caused by irritation of the sciatic nerve. While true sciatica is a form of radiating pain, lots of other issues can create a very similar sensation through referred pain.
- Sacroiliac (SI) Joint Dysfunction: Your SI joints connect your pelvis to your spine. When they get irritated or inflamed, they can refer a deep, nagging ache into the buttock, groin, and down the back of the thigh.
- Lumbar Facet Joints: These are the small joints that link your vertebrae in the lower back. If they become arthritic or injured, they can refer pain into the buttocks and the backs of the legs, though it rarely travels below the knee.
Getting this distinction right is absolutely vital for effective treatment. Treating the leg is completely pointless if the problem is coming from a joint in your lower back. Understanding https://spinebodyhealth.co.uk/what-triggers-sciatica-pain/ versus what just mimics it is the first, most important step toward getting the right help. The goal is always to trace the pain back to its real source, whether that’s a nerve, a joint, or a muscle.
Why an Accurate Diagnosis Is So Important
Referred pain is a master of disguise, which makes getting a professional diagnosis absolutely essential. Trying to treat the symptom—like massaging a sore shoulder when an irritated liver is the real issue—is like painting over a crack in the wall without checking the foundation.
It might hide the problem for a little while, but it does absolutely nothing to fix what’s actually causing it. Ignoring the pain or focusing on the wrong location can lead to serious delays in getting the right care, which is especially worrying when the source is a serious underlying condition.
The Role of a Healthcare Detective
Think of a healthcare professional as a detective piecing together a complex case. They’re trained to look beyond the obvious symptom and trace the pain back to its true origin. A thorough diagnostic process isn’t just a quick chat; it’s a methodical, multi-faceted investigation designed to uncover the root cause of your discomfort.
This process usually involves a few key steps:
- A Detailed Health History: Your practitioner will ask very specific questions about the nature of your pain, your lifestyle, and your overall health to start spotting potential patterns.
- A Comprehensive Physical Examination: This involves targeted tests to assess your movement, muscle strength, and nerve function, helping to either rule out or confirm potential sources of the pain.
- Targeted Diagnostic Tests: In some cases, imaging or other tests might be needed to get a crystal-clear picture of what's happening inside your body.
Each step provides another piece of the puzzle, allowing a professional to build a complete picture of your health. Our guide to diagnosing your pain explains this process in more detail, showing how a structured approach leads to real clarity.
The Dangers of Misinterpretation
Self-diagnosis can be incredibly misleading when it comes to referred pain. You might assume that persistent leg pain is just a simple muscle strain and try to rest it. But if that pain is actually being referred from a joint in your lower back, rest alone is never going to provide a long-term solution.
The core principle of effective treatment is to address the source, not the symptom. An accurate diagnosis ensures that your treatment plan is aimed at the right target, paving the way for lasting relief.
This diagnostic challenge contributes to a wider issue in the UK. High-impact chronic pain (HICP), which severely limits daily life, affects between 5.7% and 7.8% of adults. Referred pain can prolong this suffering by obscuring the true cause and delaying an accurate diagnosis. For conditions like back pain, which often refers pain to the legs or buttocks, the prevalence of HICP can be as high as 62.2% in some groups.
Taking your symptoms seriously and seeking a proper evaluation is the most important first step you can take. It empowers you to move past the confusion and get a clear, actionable treatment plan tailored to the real problem.
Effective Strategies for Managing Referred Pain

Once we've accurately pinpointed the true source of your discomfort, the path to lasting relief becomes much clearer. Effective management of referred pain isn’t about chasing the symptom; it's about methodically treating the underlying cause.
The goal is to move beyond simply masking the pain you feel in one area. Instead, we need to resolve the root dysfunction that’s sending those misleading signals in the first place.
This approach is fundamentally about correcting the source of the problem. If a dysfunctional joint in your spine is referring pain down your leg, the treatment must focus on restoring proper function to that specific joint. By addressing the origin, the referred symptom naturally fades away.
Building a Personalised Treatment Plan
No two people experience pain in exactly the same way. This is why a one-size-fits-all approach rarely gets the job done. A healthcare professional will develop a plan specifically for you, often combining several evidence-based strategies to get the best results.
This usually involves a combination of active and passive care. The aim is to reduce your pain, restore proper movement, and empower you with the tools to stay healthy long-term. To make sure we're on the right track, we use established outcome measures in physical therapy to help track your progress and the effectiveness of the treatment.
Core Components of Effective Management
A robust management plan often includes several key elements working together. Each component plays a distinct role in addressing the root cause and supporting your body's recovery.
Here are some of the foundational strategies we use:
- Manual Therapies: These hands-on techniques are designed to improve mobility, reduce muscle tension, and restore proper function to your joints and soft tissues. By directly addressing the source—like a stiff joint or a muscle trigger point—we can effectively "turn off" the source of the referred pain signals.
- Targeted Exercise and Rehabilitation: We prescribe specific exercises to strengthen weak muscles, stretch tight areas, and improve your overall stability. For example, core strengthening exercises provide better support for the lower back, reducing the strain on joints that might be referring pain into your buttocks or legs.
- Lifestyle and Ergonomic Adjustments: Sometimes, the source of the problem is hiding in your daily habits. A professional can help you identify and modify activities, postures, or workstation setups that contribute to your condition, stopping the issue from coming back.
The ultimate goal is not just to get you out of pain but to give you the knowledge and physical capacity to stay that way. A successful plan empowers you to take an active role in your own health and wellbeing.
The prevalence of chronic pain, including complex cases of referred pain, can vary significantly even within the UK. Detailed regional data from North Staffordshire showed that chronic pain prevalence among adults ranged from 18.6% to 50.1% across different neighbourhoods. This variation is strongly linked to socioeconomic factors, which also correlate with higher rates of musculoskeletal disorders known to cause referred pain.
Understanding these strategies is vital, especially when dealing with persistent issues that feel like sciatica. Our guide on how to prevent sciatica pain (https://spinebodyhealth.co.uk/how-to-prevent-sciatica-pain/) offers further insights into proactive measures you can take to protect your lower back.
Ultimately, partnering with a professional to create a dedicated plan is the most reliable way to find a long-term solution and regain control over your life.
Still Have Questions About Referred Pain?
Trying to make sense of referred pain can feel confusing, and it’s natural to have questions. Getting to grips with what your body is telling you is the first real step toward feeling better. Here are some clear, straightforward answers to the questions we hear most often.
How Can I Tell If My Pain Is Referred or Local?
Knowing the difference between referred and local pain is key to figuring out what’s really going on. Local pain is usually easy to understand – you sprain your ankle or get a cut, and the pain is sharp, right on the spot. It gets worse when you touch or move the injured area. Simple.
Referred pain, on the other hand, is a bit of a shapeshifter. People often describe it as a deep, dull, and widespread ache that’s frustratingly hard to pinpoint. You might struggle to show someone exactly where it hurts, and the pain can seem to come and go without any obvious reason.
Is Referred Pain Always a Sign of a Serious Problem?
Not always, but it should definitely be taken seriously. The source of referred pain can be anything from a simple tight muscle (what we call a trigger point) to a more significant issue with an internal organ.
Because the possibilities are so wide-ranging, trying to self-diagnose is never a good idea. The only way to know for sure is to get a professional evaluation. This helps rule out anything serious and gets you an accurate diagnosis for the true source of your discomfort.
The most important thing to remember is that referred pain is your body’s way of sending a signal that something isn’t right. A qualified professional can act like a detective, tracing that signal back to its origin to figure out the right course of action.
Can Stress Make Referred Pain Worse?
Absolutely. While stress doesn't actually create the nerve confusion that causes referred pain, it can certainly pour fuel on the fire. When you’re stressed, your body’s "fight or flight" response kicks in, making your entire nervous system more sensitive. This heightened state can make any existing pain feel much, much worse.
On top of that, stress often makes us tense up our muscles without even realising it. This tension can directly aggravate underlying problems—like stiff joints or muscle knots—that are already sending out referred pain signals. It quickly becomes a vicious cycle of stress and discomfort.
What Is the First Step if I Suspect Referred Pain?
If you think you might be dealing with referred pain, the single most important thing to do is book an appointment with a qualified healthcare professional. They have the expertise to carry out a proper assessment, which involves listening to your health history and doing a physical examination.
This methodical approach is the only way to accurately track down the source of your pain. A professional evaluation will give you a clear diagnosis and a sensible plan for effective treatment.
At Spine, Body & Health, our team brings a combined 38 years of experience to diagnosing and treating the root causes of pain. If you're struggling with discomfort and need clear answers, we're here to help. Schedule your consultation today by visiting us at https://spinebodyhealth.co.uk.