Stuck somewhere between your spine and your pelvis is a joint you've probably never thought much about, yet it’s one of the most important structures in your body: the sacroiliac (SI) joint. This is the crucial connection point linking the base of your spine (the sacrum) to your pelvic bones, and its main job is to act as your body’s primary shock absorber.
Understanding exactly what the sacroiliac joint is and how it works is the first step towards figuring out why it might be causing you grief.
Understanding Your Body's Shock Absorber
Imagine the keystone in a stone arch. That single stone at the very top locks everything else into place and carries an immense amount of weight. Your two SI joints, found on either side of your lower back, play a similar role, supporting your entire upper body. They form a strong, stable foundation for almost every move you make.
Now, these joints aren't like your knees or shoulders, which are built for big, obvious movements. Instead, the SI joints are designed for subtle, controlled motion—just a few millimetres here and there. This tiny bit of give is absolutely essential for absorbing the impact of walking, running, and lifting, protecting your spine from jarring forces with every step.
The Anatomy of Stability
To keep this all in check, the SI joints are reinforced by a dense network of incredibly strong ligaments. Think of them like tough, fibrous straps that hold everything together, giving your pelvis its remarkable stability and strength. This clever design ensures that forces are spread out evenly, preventing too much strain on any one part of your lower back or hips. A healthy SI joint is all about striking the perfect balance between this subtle motion and rock-solid support.
Of course, this system can’t function correctly without strong, balanced muscles surrounding the pelvis. If you want to learn more about building this essential foundation, take a look at our guide on how to strengthen core muscles. When this delicate balance gets thrown off, problems are never far behind.
The SI joint’s role in low back pain is substantial but often underestimated. Its unique structure, designed for stability over flexibility, makes it a common yet frequently overlooked source of discomfort.
To give you a clearer picture, here’s a quick summary of the SI joint's key features.
The Sacroiliac Joint At a Glance
| Characteristic | Description |
|---|---|
| Location | Where the sacrum (base of the spine) meets the iliac bones (pelvis). |
| Primary Function | Shock absorption and weight transfer between the upper body and legs. |
| Movement | Minimal, allowing for only a few millimetres of subtle motion. |
| Support | Reinforced by a dense network of strong ligaments for stability. |
| Common Issues | Dysfunction can lead to significant low back, hip, or leg pain. |
This table helps illustrate why this small joint has such a big impact on your body’s overall stability and comfort.
When the Foundation Falters
You really start to appreciate the sacroiliac joint when it stops working properly. In the UK, while true SI joint dysfunction is seen in only about 1% to 3% of the general population, it’s a major player in low back pain, accounting for up to 25% of all cases. This huge difference shows just how tricky it can be to diagnose, often getting missed because of its complex mechanics.
Things like pregnancy, carrying excess weight, or even just age-related wear and tear can increase your risk of developing SI joint problems. If you'd like to dive deeper, you can discover more insights about sacroiliac joint dysfunction in the UK on purephysiotherapy.co.uk.
Understanding this foundational joint is so important because even a minor issue can cascade into significant pain that disrupts your daily life, making simple things like standing up or climbing stairs a real challenge. This is exactly why getting an accurate diagnosis and the right treatment is vital for finding lasting relief.
Why Your SI Joints Become Painful

Pain in the sacroiliac joint rarely just shows up out of the blue. It’s almost always the result of specific triggers that knock the joint's delicate balance of stability and subtle movement off-kilter. Getting to the bottom of these root causes is the only way to find real, long-term relief because it tells us why your body’s foundation is under so much strain.
SI joint dysfunction usually boils down to one of two things: too much movement (hypermobility) or too little movement (hypomobility). Either way, the end result is inflammation, pain, and a serious disruption to your daily life.
Let’s dig into the most common reasons this happens.
Biomechanical Stress and Imbalances
Your body works like a finely tuned machine. When one part is out of alignment, it creates a domino effect that can be felt elsewhere. Biomechanical stress is a huge factor in SI joint pain, stemming from physical imbalances that overload one or both of these crucial joints.
Think of it like driving your car with one tyre that’s a bit flat. It might not seem like a big deal at first, but over time, that uneven wear puts extra strain on the axle and suspension. It’s the same with your body—seemingly small issues can create big problems for your SI joints down the line.
Common culprits we see all the time include:
- Leg Length Discrepancy: A true or functional difference in leg length can tilt your pelvis, placing uneven pressure on the SI joints with every single step you take.
- Altered Gait: An injury to your foot, ankle, or knee often changes the way you walk. This forces the SI joints to compensate and absorb forces they were never designed to handle.
- Muscle Imbalances: Weak core or glute muscles are a classic problem. If they aren’t doing their job to support the pelvis, the SI joints are left vulnerable to excessive strain and instability.
Hormonal Changes and Increased Laxity
Hormonal shifts can have a massive impact on the ligaments holding your pelvis together. This is especially noticeable during pregnancy when the body releases a hormone called relaxin.
Relaxin’s job is to increase the laxity of the pelvic ligaments to prepare the body for childbirth. While it’s a completely natural and necessary process, it can temporarily make the SI joints less stable, leaving them wide open to irritation and pain.
For many women, this increased joint mobility is a primary contributor to lower back and pelvic girdle pain during and after pregnancy. While the ligaments typically tighten again after childbirth, sometimes the joint remains unstable, leading to chronic discomfort.
This hormonal influence is a key reason why women are generally more prone to experiencing SI joint issues than men. Their pelvic structure is built for more flexibility, which can sometimes come at the cost of stability.
The Impact of Trauma and Degeneration
Sometimes, the cause of SI joint pain is much more direct and obvious. A sudden, forceful impact can easily injure the ligaments around the joint, triggering immediate dysfunction and inflammation.
A hard fall onto your bum, a car accident, or even a misstep while playing sport can jolt the joint, either making it unstable or locking it in the wrong position. This kind of traumatic event often causes a sharp, localised pain that’s impossible to ignore.
Over the long haul, degenerative conditions can also take their toll. Just like any other joint, the SI joint is vulnerable to wear-and-tear arthritis (osteoarthritis). As the protective cartilage slowly wears away, the bones can start rubbing against each other, causing inflammation, stiffness, and chronic pain. This slow, progressive damage is a very common factor for older adults struggling with persistent low back and hip discomfort.
Recognising the Symptoms of SI Joint Pain
Sacroiliac joint pain is a notorious mimic, often disguising itself as other common back problems. Its symptoms can be so varied and widespread that many people struggle for years without a clear diagnosis. Learning to recognise the unique signs of SI joint trouble is the first, most important step toward getting the right help.
The classic symptom is a deep, nagging ache felt in the lower back or buttock, usually on one side. This isn't just a surface-level muscle ache; it feels like it's coming from deep within the pelvis. But the discomfort rarely stays in one place.
The Tell-Tale Signs of Dysfunction
One of the most confusing aspects of SI joint pain is its ability to travel. The pain often radiates into the groin, hip, or down the back of the thigh, which frequently leads to a misdiagnosis of sciatica. But there's a key difference. True sciatica typically involves nerve-related sensations like tingling, numbness, or weakness that can extend all the way to the foot.
In contrast, SI joint pain that radiates is a type of referred pain, where the brain perceives discomfort in an area different from the actual source. You can explore more about what referred pain is in our detailed article. This distinction is crucial for an accurate diagnosis and effective treatment.
Beyond the radiating ache, other symptoms point directly to the SI joint as the culprit:
- Sharp, Stabbing Pain: You might feel a sudden, sharp pain when you put weight on one leg, like when climbing stairs, rolling over in bed, or getting out of a car.
- A Feeling of Instability: Many people describe a sensation that their pelvis is "giving way" or feels unstable when standing, walking, or moving from sitting to standing.
- Stiffness and Discomfort: The pain and stiffness often feel worst after sitting or standing for a long time and can be most intense first thing in the morning.
How SI Joint Pain Manifests in Daily Life
Understanding the textbook symptoms is one thing, but recognising how they impact your daily activities is what really brings it home. The discomfort from a dysfunctional sacroiliac joint isn't just a vague backache; it's a specific set of triggers that can make simple tasks feel monumental.
See if any of these common scenarios sound familiar:
- Difficulty Sitting: Prolonged sitting, especially on hard surfaces or while driving, can become unbearable. You might find yourself constantly shifting your weight to find a position that doesn’t hurt.
- Pain with Transitional Movements: The simple act of rising from a chair can trigger a sharp, localised pain deep in your buttock or lower back.
- Uneven Weight Distribution: You may notice that you lean to one side when standing to take pressure off the painful joint, often without even realising you're doing it.
One of the most defining characteristics of SI joint pain is how it flares up during activities that load the joint asymmetrically. This includes actions like climbing stairs, running, or even standing on one leg to put on your trousers.
In the UK, sacroiliac joint dysfunction (SIJD) is a significant factor in lower back pain cases, affecting an estimated 15% to 30% of patients. Some studies suggest this figure could be as high as 33% among those presenting with lower back problems. It's particularly noteworthy that women are disproportionately affected compared to men, a trend that aligns with broader UK health data on musculoskeletal conditions.
Ultimately, if your pain is concentrated just below your belt line, gets worse with specific movements, and feels more like a deep pelvic issue than a muscle strain, your SI joint could be the source. Empowering yourself with this knowledge is key to seeking an accurate diagnosis and finally getting on the path to lasting relief.
How SI Joint Dysfunction Is Accurately Diagnosed
Getting the right diagnosis for sacroiliac joint pain is the crucial first step toward lasting relief. Because its symptoms so often mimic other back, hip, and leg problems, pinning down the SI joint as the true culprit requires a careful, thorough investigation. It’s a process that combines your personal experience with an expert clinical assessment.
The journey always begins with a detailed conversation. A specialist will want to know exactly what you’re feeling, what makes the pain better or worse, and how it’s affecting your day-to-day life. This isn't just a chat; it's a vital part of the puzzle, providing clues that either point towards or away from the SI joint.
This initial discussion helps us build a picture of your symptoms and see how they match up with common patterns of SI joint dysfunction.
The chart below shows the most common symptoms reported by people with confirmed SI joint issues, and it really highlights how varied the pain can be.
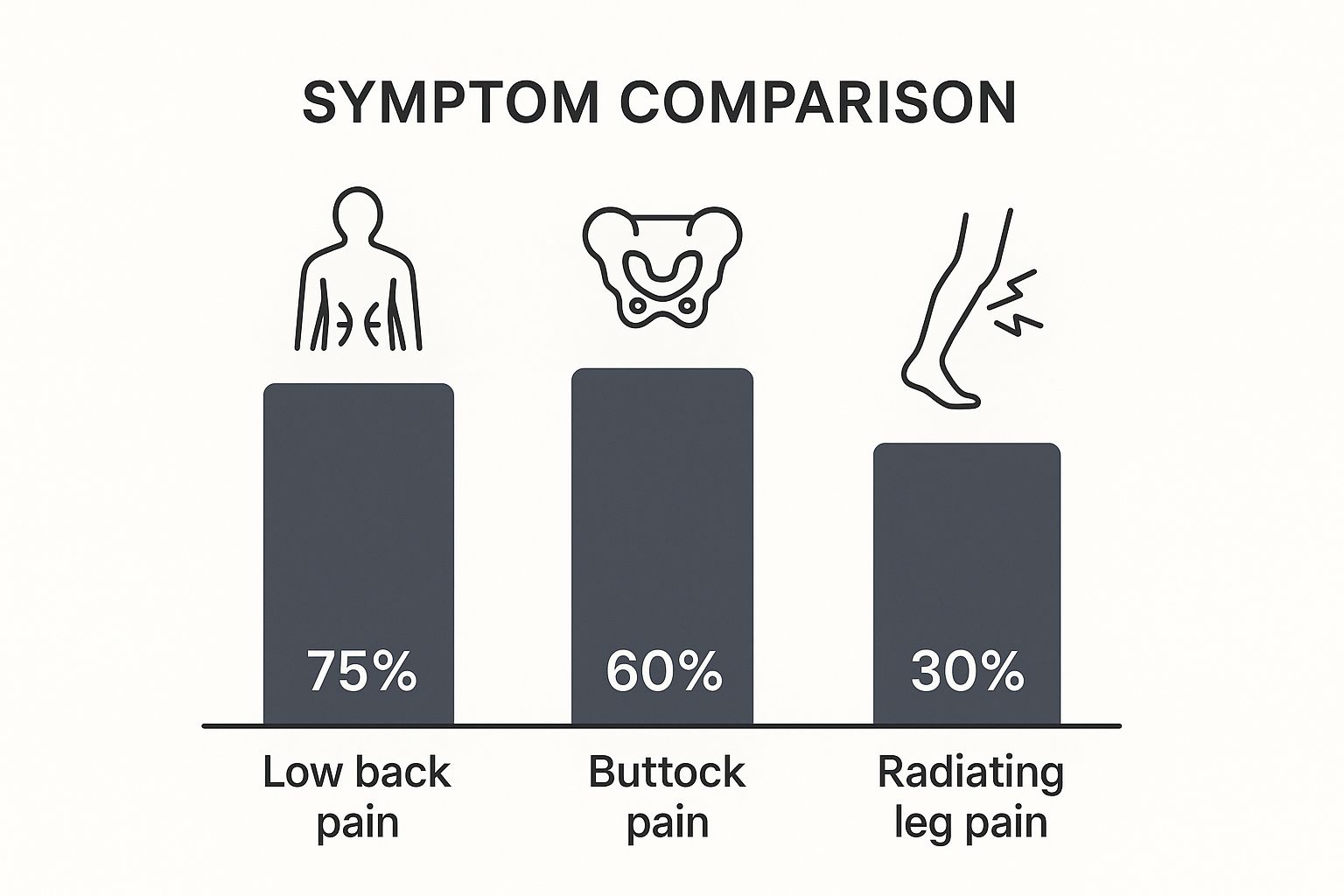
As you can see, while low back pain is the most frequent complaint, a huge number of people also get pain deep in the buttock and even down the leg.
The Hands-On Physical Examination
After our chat, we move on to a hands-on physical exam to assess your movement, posture, and muscle strength. We'll observe how you walk, stand, and sit, looking for subtle imbalances like a tilted pelvis or even a slight difference in leg length that could be putting your SI joints under constant strain.
This exam is about more than just looking. It involves feeling for tenderness directly over the sacroiliac joint itself. By pressing on specific points around your lower back and pelvis, a specialist can often replicate the exact pain you've been living with—a strong indicator that the SI joint is involved.
Isolating the Pain with Provocation Tests
To really zero in on the SI joint, specialists use a series of specific movements known as orthopaedic provocation tests. These are simple, hands-on tests where a practitioner gently stresses the joint through various positions to see if they reproduce your familiar pain.
Think of these tests like trying to find a squeaky floorboard. You press on different spots until you find the one that makes the noise. Provocation tests work the same way, applying targeted pressure to isolate the pain and confirm the SI joint is the culprit.
For a diagnosis of SI joint dysfunction to be strongly considered, at least three of these tests need to be positive—meaning they successfully recreate your specific pain. It's a highly reliable method for telling the difference between true SI joint pain and other lower back problems.
The Role of Imaging Studies
While the physical tests are key, imaging like X-rays or MRIs also plays an important, though often secondary, role. An X-ray might be used to check for signs of arthritis or other structural changes in the bones of your pelvis and spine.
An MRI, on the other hand, gives us a much more detailed look at the soft tissues, like the ligaments and cartilage around the SI joint. While an MRI doesn't always show obvious signs of dysfunction, it is incredibly useful for ruling out other potential causes of your pain, such as a herniated disc, nerve compression, or a problem with your hip.
Comparing Diagnostic Approaches for SI Joint Pain
To understand how these different methods fit together, here’s a quick overview of what each one brings to the diagnostic process.
| Diagnostic Method | Purpose | What It Shows |
|---|---|---|
| Patient History | To understand the patient's unique symptoms and how they affect daily life. | Pain patterns, triggers, and the personal impact of the discomfort. |
| Physical Examination | To assess posture, movement, muscle strength, and locate tenderness. | Pelvic imbalances, muscle weakness, and tenderness directly over the SI joint. |
| Provocation Tests | To specifically stress the SI joint to see if it reproduces the familiar pain. | A positive test strongly suggests the SI joint is the source of the pain. |
| Imaging (X-ray/MRI) | To visualise the bones and soft tissues of the pelvis and spine. | Signs of arthritis, structural changes, or helps rule out other issues like disc herniations. |
| Diagnostic Injection | To confirm the diagnosis by numbing the joint and seeing if the pain disappears. | Conclusive proof that the SI joint is the pain generator. |
Each of these steps provides another layer of information, helping us build a complete and accurate picture of what's going on.
The Gold Standard: Diagnostic Injection
When the diagnosis is still not 100% clear after the physical exam and imaging, the definitive test is a fluoroscopically-guided diagnostic injection. This is a highly precise procedure where a local anaesthetic is injected directly into the sacroiliac joint using real-time X-ray guidance (fluoroscopy).
The logic is beautifully simple: if numbing the joint makes the pain vanish, we have conclusive proof that the SI joint is the source of the problem. A significant reduction in pain—typically 75% or more—is considered a positive result, confirming the diagnosis with a very high degree of certainty. This step doesn't just give us a final answer; it clears the path for planning a targeted and truly effective treatment.
Effective Treatment Pathways For Lasting Relief
True recovery from sacroiliac joint pain isn't about masking symptoms with temporary fixes. Lasting relief comes from a proper strategy that gets to the root cause of the dysfunction, restoring balance and stability to your whole pelvic region. The process almost always starts with foundational, non-invasive therapies designed to calm inflammation and correct the biomechanical hitches that led to the pain in the first place.
This progressive approach means we start with the simplest, most effective methods before even thinking about more direct interventions. The goal is to build a strong, resilient foundation that supports your SI joint for the long haul.
Building Stability With Targeted Therapy
The cornerstone of getting the SI joint sorted is targeted physical therapy. This isn't just a random list of back exercises; it's a precise plan to correct muscle imbalances, strengthen weak supporting muscles, and get your pelvis properly aligned again. A specialist will guide you through exercises that specifically target your core, glutes, and pelvic floor muscles—the very muscles in charge of stabilising your sacroiliac joint.
Alongside strengthening, specialised manual therapy techniques can be incredibly effective. These hands-on methods help to gently mobilise a stiff or "stuck" joint, or stabilise one that has become too loose. By tackling both movement and stability, we can start to retrain your body to move correctly, taking that excessive strain off the SI joint. It’s important to find the right professional for your needs, and you can learn more about the distinctions between physiotherapy and other manual therapies in our guide.
For anyone looking for lasting relief from SI joint pain, sorting out your sleep environment can also be a game-changer. This includes looking into options like finding the best memory foam mattress for superior comfort and pressure relief.
Interventional Options For Healing And Control
When the foundational therapies aren't quite enough to break the cycle of pain and inflammation, more direct interventions might be needed. These options are designed to get severe symptoms under control and create a window of opportunity for your physical therapy to really work.
One common approach is a therapeutic SI joint injection. Unlike a diagnostic injection, this procedure uses a corticosteroid to deliver powerful anti-inflammatory medication right to the source of the pain. It can provide significant, though sometimes temporary, relief.
An effective therapeutic injection can calm the joint enough to allow you to engage fully in your rehabilitation programme, turning a vicious cycle of pain and immobility into a virtuous cycle of recovery and strengthening.
On top of that, regenerative treatments are gaining real recognition for their ability to kick-start natural healing within the joint and its supporting ligaments. These procedures use your body's own healing agents to help repair damaged tissues, addressing the root cause of the instability and pain.
Our Integrated Approach To Your Recovery
Here at our clinic, we are firm believers that the most effective path to recovery is an integrated one, combining precise diagnostics with a truly personalised treatment plan. We don't do "one-size-fits-all." Instead, we start by pinpointing the exact cause of your sacroiliac dysfunction—whether it's instability, stiffness, or inflammation.
From there, we build a multi-faceted plan tailored to your specific needs. This might include:
- Advanced Diagnostics: Using a combination of physical assessment and, when needed, imaging to get a crystal-clear picture of your joint's health.
- Manual Therapy: Employing hands-on techniques to restore proper joint mechanics and get you out of pain.
- Targeted Rehabilitation: Designing a specific exercise programme to strengthen the muscles that support the joint and prevent future flare-ups.
- Regenerative Treatments: Using your body's own healing power to repair damage and provide long-term stability.
In some severe cases where conservative treatments don't bring relief, surgical options like SI joint fusion might be considered. This procedure aims to permanently stabilise the joint. In the UK, data shows that between 2010 and 2021, around 18,000 patients had this surgery. Interestingly, females made up approximately 70% of these cases, with a mean age of about 51 years, highlighting a specific group where this intervention has become more common. You can read the full nationwide analysis of sacroiliac joint fusion trends on londonspine.com to delve into the details.
Our integrated strategy is designed to move you beyond temporary fixes. By addressing the root cause of your pain with a comprehensive and personalised plan, we can help you find a path to meaningful, long-term relief and get you back to living your life without limitations.
Frequently Asked Questions About SI Joint Pain

It’s completely normal to have questions when you’re dealing with something as disruptive as sacroiliac joint pain. Getting clear answers is the first step toward understanding what’s happening in your body and how to move forward. Below, we’ve answered some of the most common queries we hear from patients.
How Can I Differentiate SI Joint Pain From Sciatica?
This is a big one, and the confusion is understandable. The main difference really comes down to where the pain is and what it feels like.
SI joint pain is typically a deep, localised ache you’ll feel around your low back, buttock, or sometimes the groin. While that ache can sometimes refer down the back of your thigh, it rarely travels past the knee. Sciatica, on the other hand, is classic nerve pain—think tingling, numbness, or a sharp, shooting sensation that can zip all the way down your leg to your foot.
Can Lifestyle Changes Help With Sacroiliac Pain?
Without a doubt. In fact, lifestyle adjustments are a cornerstone of effective, long-term management of SI joint dysfunction. We always emphasise targeted exercises to strengthen the core and gluteal muscles, as these provide the crucial support the joint needs to function without pain.
Things like adopting an anti-inflammatory diet can also help calm down inflammation throughout your body. And, of course, maintaining a healthy weight is vital—it simply reduces the day-to-day mechanical load on your sacroiliac joints.
Recovery is rarely a single solution. It is the combination of targeted physical therapy, mindful daily habits, and appropriate lifestyle modifications that creates the most powerful and lasting relief from sacroiliac pain.
How Long Does Recovery From SI Joint Dysfunction Take?
The honest answer is that it varies hugely from one person to the next, depending on the root cause and how severe the issue is. With a dedicated physical therapy programme, many patients report a huge improvement in their symptoms within 6 to 12 weeks.
However, if it’s a chronic issue or involves significant joint instability, it will likely require a longer-term management plan to keep things stable and prevent flare-ups. We also know patients often have questions about the financial side of treatment; for instance, you can learn more about specific aid like Medicare coverage for orthotics.
Is It Safe To Continue Exercising?
This is a great question, and the answer is a classic: it depends. Low-impact activities are often fantastic. Things like swimming, gentle cycling, or walking can strengthen the supporting muscles without jarring the joint.
On the flip side, high-impact exercises—running or heavy lifting, for example—should usually be avoided, especially when you’re in the middle of a flare-up. They can easily worsen the inflammation and pain. The most important thing is to consult a specialist who can give you personalised advice on which movements are safe and genuinely beneficial for your specific situation.
Ready to find the root cause of your pain and get a personalised plan for lasting relief? At Spine, Body & Health, our specialists combine advanced diagnostics with effective treatment strategies to help you get back to living a pain-free life. Book your consultation today by visiting us at https://spinebodyhealth.co.uk.




